Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (26 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
10.95Mb size Format: txt, pdf, ePub
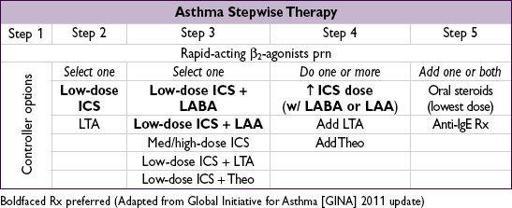
• Education and avoidance of environmental triggers for all Pts; yearly flu shot • Use quick-relief rescue medication as needed for all Pts • Goal to achieve
complete control
= daily sx ≤2/wk, Ø nocturnal sx or limitation of activity, reliever med ≤2/wk, nl PEF or FEV
1
; partly controlled = 1–2 of the above present in a wk; uncontrolled = ≥3 of the above present in a wk • Step up treatment as needed to gain control, step down as tolerated • If PEF ↓ 15% × 2 d or ↓ 30%, 4× ICS dose ↓ need for PO steroids (
AJRCCM
2009;180:598) • Variants in glucocorticoid-induced transcript 1 gene a/w resp to ICS (
NEJM
2011;365:1173)
EXACERBATION
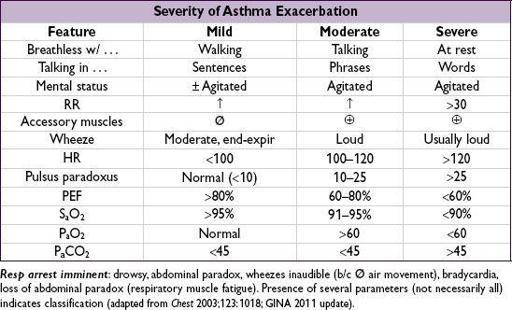
Evaluation
• History: baseline PEF, steroid requirement, ED visits, hospital admissions, prior intubation Current exacerbation: duration, severity, potential precipitants, meds used
Risk factors for life-threatening
: prior intubation, h/o near-fatal asthma, ED visit/hosp for asthma w/in 1 y, current/recent PO steroids, not using ICS, overdependent on SABA, Ψ, h/o noncompl
• Physical exam: VS, pulm, accessory muscle use, pulsus paradoxus, abdominal paradox
Assess for barotrauma: asymmetric breath sounds, tracheal deviation, subcutaneous air → pneumothorax, precordial (Hamman’s) crunch → pneumomediastinum
• Diagnostic studies:
PEF
(used to follow clinical course);
S
a
O
2
;
CXR
to r/o PNA or PTX ABG if severe: low P
a
CO
2
initially; nl or high P
a
CO
2
may
signify tiring
Initial treatment
(
NEJM
2010;363;755)
•
Oxygen
to keep S
a
O
2
≥90%
•
Inhaled SABA
(eg, albuterol) by MDI (4–8 puffs) or nebulizer (2.5–5 mg) q20min •
Corticosteroids
: prednisone 0.5–1 mg/kg PO; IV if impending resp arrest •
Ipratropium
MDI (4–6 puffs) or nebulizer (0.5 mg) q20min if severe (
Chest
2002;121:1977) • Epinephrine (0.3–0.5 mL SC of 1:1000 dilution) no advantage over inh SABA • Montelukast IV ↑ FEV
1
but did not Δ rate of hosp (
J Allergy Clin Immunol
2010;125:374) •
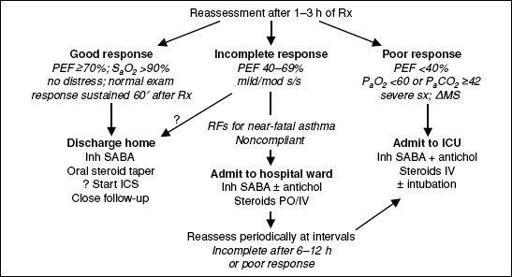
Reassess after 60–90 min of Rx
Mild-mod exacerbation: cont SABA q1h
Severe exacerbation: SABA & ipratropium q1h or continuously; ± Mg 2 g IV over 20 min (
Lancet
2003;361:2114); ± heliox (60–80%)
•
Decide disposition within 4 h of presentation and after
1–3 h of Rx
Figure 2-2
Disposition of patients after initial treatment of asthma exacerbation
ICU-level care
•
High-dose steroids
: methylprednisolone 125 mg IV q6h (
Archives
1983;143:1324) •
Invasive ventilation
:
large ET tube, P
plat
<30 cm H
2
O (predicts barotrauma better than PIP), max exp time
PEEP individualized to Pt physiology
paralysis, inhalational anesthetics, bronchoalveolar lavage w/ mucolytic, heliox (60–80% helium) and ECMO have been used with success
• NPPV likely improves obstruction (
Chest
2003;123:1018), but controversial and rarely used
ANAPHYLAXIS
Definition and pathophysiology (
Ann Emerg Med
2006;47:373)
• Severe, rapid-onset (mins to hrs), potentially life-threatening systemic allergic response • IgE-mediated mast cell degranulation with release of histamine, tryptase and TNF
• Precipitates systemic reactions (bronchospasm, tissue swelling, fluid shifts, vasodilation) • Common triggers: penicillins, cephalosporins, shellfish, nuts, insect stings, IV contrast (not truly an IgE-mediated mechanism, but clinically similar)
Diagnosis:
any of the three following criteria
1) Acute illness with skin ± mucosal involvement (rash, flushing, hives), AND at least one of:
• Respiratory compromise (wheeze, stridor, dyspnea, hypoxemia)
• Hypotension or hypoperfusion (syncope, incontinence)
2) Two or more of the following after exposure to a
likely
allergen: skin/mucosal involvement, respiratory compromise, ↓ BP or hypoperfusion, GI symptoms 3) Hypotension after exposure to
known
allergen for that Pt
Treatment
•
Epinephrine
: IM or SC 0.3–0.5 mL of 1:1000 dilution (1 mg/mL) q5–20min; if HoTN or cardiac arrest, IV (or via ETT) 2.5–10 mL of 1:10,000 dilution q5min ± gtt •
Airway management
: suppl O
2
± intubation (or cricothyroidotomy if laryngeal edema) β
2
-agonists (stacked or continuous nebulizers) for refractory bronchospasm • Fluid resuscitation w/ lg volume of crystalloid (may extravasate up to 35% of blood volume) • Antihistamines relieve hives & itching,
no effect on airway or hemodynamics
H1RA (diphenhydramine 50 mg IV/IM) ± H2RA (eg, ranitidine 50 mg IV) • Corticosteroids have no immediate effect but may help prevent relapse: methylprednisolone 125 mg IV q6h if severe or prednisone 50 mg PO
• Glucagon (1–5 mg IV over 5 min) if inotropic or chronotropic support needed in Pt taking bB
• Avoid unopposed a-adrenergic vasopressors
Disposition
• Mild rxn limited to urticaria or mild bronchospasm can be observed for ≥6 h; admit all others • Watch for biphasic reaction; occurs in 23%, typically w/in 8–10 h but up to 72 h
• At time of d/c: education re: allergen avoidance, instruction and Rx for EpiPen, allergist f/u
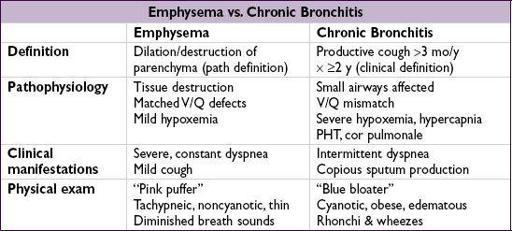
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
Definition and epidemiology
(
NEJM
2004;350:26)
• Progressive airflow limitation caused by airway and parenchymal inflammation
Pathogenesis
(
Lancet
2003;362:1053)
•
Cigarette smoke
(centrilobular emphysema, affects 15–20% of smokers)
• Recurrent airway infections
• ɑ
1
-antitrypsin defic.: early-onset panacinar emphysema, 1–3% of COPD cases. Suspect if age <45, lower lungs affected, extrathoracic manifestations (liver disease [not if MZ subtype], FMD, pancreatitis). ✓ serum AAT level (nb, acute phase reactant).
Clinical manifestations
• Chronic cough, sputum production, dyspnea; later stages → freq exac., a.m. HA, wt loss
• Exacerbation triggers: infxn, other cardiopulmonary disease, incl. PE (
Annals
2006;144:390)
Infxn: overt tracheobronchitis/pneumonia from viruses,
S. pneumoniae
,
H. influenzae
,
M. catarrhalis
or triggered by changes in strain of colonizers (
NEJM
2008;359:2355)
• Physical exam: ↑ AP diameter of chest (“barrel-chest”), hyperresonance, ↓ diaphragmatic excursion, ↓ breath sounds, ↑ expiratory phase, rhonchi, wheezes during exacerbation: tachypnea, accessory muscle use, pulsus paradoxus, cyanosis
Diagnostic studies
• CXR (see Radiology inserts): hyperinflation, flat diaphragms, ± interstitial markings & bullae
• PFTs:
Obstruction
: ↓↓ FEV
1
, ↓ FVC,
FEV
1
/FVC <0.7 (no sig
Δ
post bronchodilator)
, expiratory scooping of flow-volume loop;
Hyperinflation
: ↑↑ RV, ↑ TLC, ↑ RV/TLC;
Abnormal gas exchange
: ↓ D
L
CO (in emphysema)
• ABG: ↓ P
a
O
2
, ± ↑ P
a
CO
2
(in chronic bronchitis, usually only if FEV
1
<1.5 L) and ↓ pH
• ECG: PRWP, S1S2S3, R-sided strain, RVH, ↑ P waves in lead II (“P pulmonale”)
Chronic treatment
(
NEJM
2010;362:1407;
Lancet
2012;379:1341)
Other books
Jericho (A Redemption Novel) by Ginger Jamison
Bar Mate by Rebecca Royce
Fast Lane by Dave Zeltserman
My Best Friend's Ex by Tina Gayle
The Good Wife by Elizabeth Buchan
The Dark Light by Julia Bell
Futures and Frosting by Tara Sivec
Waiting for Morning by Karen Kingsbury
Dystopia: YA Paranormal Adventure Romance by Ergo, Anthony
Paradise - Part Four (The Erotic Adventures of Sophia Durant) by Casper, O.L.