Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (25 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
2.76Mb size Format: txt, pdf, ePub
• Duplex arterial U/S; CTA w/ distal run-off; MRA or angio
Treatment (
JACC
2013;61:1555; JAMA 2013;309:453)
• Risk factor modification. Supervised exercise Rx. Screen for CAD.
• Cilostazol (if no HF) & ? ACEI to ↓ sx. ASA or clopi to ↓ D/MI/stroke if claud. or ABI <0.9.
• Revasc if CLI or limiting/refractory claudication
Acute limb ischemia (ALI)
• Sudden decrement in limb perfusion that threatens viability;
viable
(no immed threat of tissue loss): audible art. Doppler signals, sensory & motor OK
threatened
(salvage requires prompt Rx): loss of arterial Doppler signal, sensory or motor
• Etiologies: embolism > acute thrombosis (eg, athero, APLA, HITT), trauma to artery
• Clinical manifestations (
6 Ps
): pain (distal to proximal, ↑ in severity), poikilothermia, pallor, pulselessness, paresthesias, paralysis
• Testing: thorough pulse & neuro exam; arterial Doppler; angiography, either CT w/ bilateral run-off through feet or arteriography
• Urgent consultation w/ vascular medicine and/or vascular surgery
• Treatment: immediate anticoagulation ± intraarterial lytic; angioplasty or surgery
NOTES
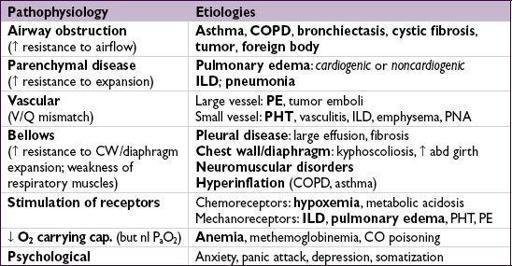
DYSPNEA
Evaluation
• History: quality of sensation, tempo, positional dependence, exac./allev. factors, exertion
• Cardiopulmonary exam, S
a
O
2
, CXR (see Appendix & Radiology inserts), ECG predictors of CHF: h/o CHF, PND, S
3
, CXR w/ venous congestion, AF (
JAMA
2005;294:1944) dyspnea w/ nl CXR → CAD, asthma, PE, PHT, early ILD, anemia, acidosis, NM disease
• Based on results of initial evaluation: PFT, chest CT, TTE, cardiopulmonary testing
•
BNP & NT-proBNP
↑ in CHF (also ↑ in AF, RV strain from PE, COPD flare, PHT, ARDS) BNP <100 pg/mL to r/o CHF (90% Se), >400 to r/i (
NEJM
2002;347:161)
NT-proBNP <300 pg/mL to r/o CHF (99% Se); age-related cut points to r/i: >450 pg/mL (<50 y), >900 (50–75 y), >1800 (>75 y) (
EHJ
2006;27:330)
↑ in chronic heart failure, ∴ need to compare to known “dry BNP”
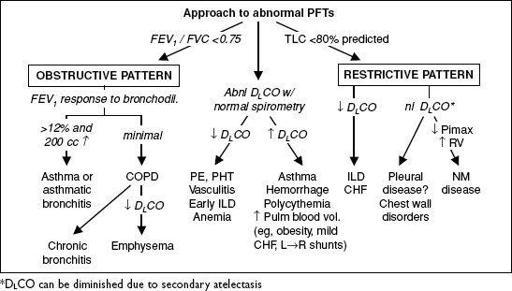
PULMONARY FUNCTION TESTS (PFTs)
•
Spirometry
: evaluate for obstructive disease
Flow-volume loops: diagnose and/or localize obstruction
Bronchodilator: indicated if obstruction at baseline or asthma clinically suspected
Methacholine challenge: helps dx asthma if spirometry nl, >20% ↓ FEV
1
→ asthma
•
Lung volumes
: evaluate for hyperinflation or restrictive disease including NM causes •
D
L
CO
: evaluates functional surface area for gas exchange; helps differentiate causes of obstructive and restrictive diseases and screens for vascular disease & early ILD
Figure 2-1 Approach to abnormal PFTs
ASTHMA
Definition and epidemiology
• Chronic inflam. disorder w/
airway hyperresponsiveness
+
variable airflow obstruction
• Affects
5% population;
85% of cases by age 40 y
Clinical manifestations
(
NEJM
2001;344:350)
• Classic triad =
wheezing
,
cough and dyspnea
; others include chest tightness, sputum; symptoms typically
chronic
with
episodic exacerbation
• Precipitants (
triggers
)
respiratory irritants
(smoke, perfume, etc.) &
allergens
(pets, dust mites, pollen, etc.)
infections
(URI, bronchitis, sinusitis)
drugs
(eg, ASA & NSAIDs via leukotrienes, bB via bronchospasm, MSO
4
via histamine) emotional stress, cold air, exercise (increase in ventilation dries out airways)
Physical examination
• Wheezing and prolonged expiratory phase • Presence of nasal polyps, rhinitis, rash →
allergic component
• Exacerbation → ↑ RR, ↑ HR, accessory muscle use, diaphoresis, pulsus paradoxus
Diagnostic studies
•
Peak exp flow
(
PEF
): ≥60 L/min ↑ after bronchodil or ≥20% diurnal variation c/w asthma. <80% personal best c/w poor control, <50% c/w severe exacerbation.
•
Spirometry
: ↓ FEV
1
, ↓ FEV
1
/FVC, coved flow-volume loop; lung volumes: ± ↑ RV & TLC
bronchodilator response (↑ FEV
1
≥12% & ≥200 mL) strongly suggestive of asthma methacholine challenge (↓ FEV
1
≥20%) if PFTs nl: Se >90% (
AJRCCM
2000;161:309)
• Sputum: eos >3% has 86% Se, 88% Sp; can also see
Curschmann’s spirals
(mucus casts of distal airways) and
Charcot-Leyden
crystals (eosinophil lysophospholipase) • Allergy suspected → consider ✓ serum IgE, eos, skin testing/RAST
Ddx
(“all that wheezes is not asthma … ”)
• Hyperventilation & panic attacks • Upper airway obstruction or inh foreign body; laryngeal/vocal cord dysfxn (eg, 2° to GERD) • CHF (“cardiac asthma”); COPD, bronchiectasis; ILD (including sarcoidosis); vasculitis; PE
“Asthma plus” syndromes
(
Lancet
2002;360:1313)
• Atopy = asthma + allergic rhinitis + atopic dermatitis • ASA-sensitive asthma (Samter’s syndrome) = asthma + ASA sensitivity + nasal polyps • ABPA = asthma + pulmonary infiltrates + allergic rxn to
Aspergillus
• Churg-Strauss = asthma + eosinophilia + granulomatous vasculitis
“Reliever” medications
(used prn to quickly relieve sx)
•
Short-acting
inh β
2
-agonists
(SABA): albuterol Rx of choice •
Short-acting
inh
anticholinergics
(ipratropium) ↑ β
2
-agonist delivery → ↑ bronchodilation
“Controller” meds
(taken daily to keep control)
(
NEJM
2009;360:1002)
• Inh
corticosteroids
(ICS): Rx of choice (
JAMA
2001;285:2583). PRN ? as good as daily for mild asthma (
NEJM
2005;352:1519 & 2007;356:2040). PO steroids may be needed for severely uncontrolled asthma, but avoid if possible b/c systemic side effects.
•
Long-acting
inh β
2
-
agonists
(LABA; eg, salmeterol): ↑ PEF when added to ICS (
Lancet
2009;374:1754). Except for exercise-induced asthma, should
not
be used w/o ICS (may ↑ mortality, esp. in African Americans) (
Chest
2006;129:15;
Annals
2006;144:904). Clinical relevance of β
2
-receptor pharmacogenetic interaction not validated (
Lancet
2009;374:1754).
•
Long-act
inh
anticholinergics
(LAA; eg, tiotropium): add-on if sx despite ICS (superior to ↑ ICS,to adding LABA;
NEJM
2010;363:1715) or if sx despite ICS+LABA (
NEJM
2012;367:1198) •
Nedocromil/cromolyn
: limited use in adults. Useful in young Pts, exercise-induced bronchospasm; ineffective unless used before trigger or exercise exposure.
•
Theophylline
: useful if hard to control sx; PO convenient, but high side-effect profile •
Leukotriene antagonists
(LTA): some Pts very responsive, esp. ASA-sens (
AJRCCM
2002;165:9) and exercise-induced (
Annals
2000;132:97). May be noninf to ICS initial Rx and LABA add-on Rx (
NEJM
2011;364:1695).
•
Anti-IgE
: for uncontrolled mod-to-severe allergic asthma (↑ IgE) on ICS ± LABA (
NEJM
2006;354:2689;
Annals
2011;154:573); not cost-effective for most Pts (
JACI
2007;120:1146)
Other
• Behavior modification: identify and avoid triggers; PPI w/o benefit (
NEJM
2009;360:1487) • Immunotherapy (eg, desensitization): may be useful if significant allergic component • TNF antagonists may be helpful in Pts w/ refractory asthma (
NEJM
2006;354:697) • Anti-IL5 (mepolizumab) ↓ exac. w/ sev asthma (
Lancet
2012;380:651), not yet FDA approved • Anti-IL13 (lebrikizumab) ↑ FEV
1
(
NEJM
2011;365:1088), not yet FDA approved • Bronchial thermoplasty (exp’tal): radiofrequency destruction of airway smooth muscle no Δ in FEV
1
, but ↓ in sx and # of exacerbations (
NEJM
2007;356:1327)
Principles of treatment
Other books
Rewind (Vanish Book Three) by Daise, Sonny
Heart to Heart by Lurlene McDaniel
Out on a Limb by Gail Banning
Unbound Pursuit by Lindsay McKenna
Las cenizas de Ovidio by David Wishart
Scarlett by Ripley, Alexandra
Beginning of Forever (Heaven Hill #7) by Laramie Briscoe
Not Quite Terran Part 1 (Scifi Alien Romance Serial) by Erin Tate
The Wrong Man by Lane Hayes
Shelby by McCormack, Pete;