Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (82 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
8.34Mb size Format: txt, pdf, ePub
• Reasons for failure to improve on initial Rx:
Insufficient time: may take ≥72 h to see clinical improvement
Insufficient drug levels: eg, vanco trough <15–20 µg/mL (needed for lung penetration)
Resistant organisms (or superinfxn): eg, MRSA,
Pseudomonas
; consider
bronchoscopy
Wrong dx: fungal/viral, chemical pneumonitis, PE, CHF, ARDS, DAH, ILD;
consider CT
Parapneumonic effusion/empyema/abscess: esp. seen w/ strep; if CXR,
consider CT
(dx tap ± chest tube if effusion present, esp. if loculated)
Metastatic infection (eg, endocarditis, meningitis, arthritis)
Prognosis
• Pneumonia and influenza are the 8th leading cause of death in the U.S.
• For low-risk Pts, can discharge immediately after switching to PO abx (
CID
2007;44:S27) • CXR resolves in most by 6 wk; consider f/u to r/o underlying malignancy (esp. if age >50 y or smoker,
Archives
2011;171:1192) or other dx • Severe CAP (generally requiring ICU) defined as: septic shock, resp failure, or ≥3 of: RR ≥30, P
a
O
2
/F
i
O
2
≤250, <36°C, HoTN, DMS, multilobar, WBC <4k, plt <100, BUN ≥19.9, metabolic acidosis, ↑ lactate (ATS/IDSA criteria,
CID
2007;44:S27) •
SMART-COP
risk score:
S
BP <90 (2 points),
M
ultilobar infiltrates,
A
lb <3.5 g/dL,
R
R ≥30,
T
achycardia (HR >125),
C
onfusion,
O
2
sat <90% (2 points), arterial
p
H <7.35 (2 points) score ≥3 points has Se ~60–90% & Sp 45–75% for need for ICU care (
CID
2008;47:375)
Prevention
• Pneumococcal vaccine (PPSV23):
all
persons >65 y of age. If high-risk comorbidity, give at younger age and consider additional vaccination with PCV13.
• VAP precautions: HOB >30°, chlorhexidine rinse; aspiration precautions in high-risk Pts • Tdap booster: 1 time dose in adults with uncertain vaccination history (
MMWR
2012; 61:468)
VIRAL RESPIRATORY INFECTIONS
URI, bronchitis, bronchiolitis, pneumonia
(
Lancet
2011;377:1264)
Microbiology & epidemiology
• Typical pathogens: short, mild = rhinovirus, coronavirus; longer, more severe or complicated =
influenza
, parainfluenza, respiratory syncytial virus (RSV), adenovirus, metapneumovirus. Can be esp. severe in immunosupp.
• Seasonal flu: 365,000 hosp, 51,000 deaths per y in U.S.; most >65 y (
NEJM
2008;359:2579) • Pandemic 2009 H1N1 (swine): more severe in younger and obese Pts (
JAMA
2009;302:1896) • Sporadic 2011 H3N2: adults exposed to swine (also human-to-human) (
MMWR
2011;60:1615) • H5N1 influenza (avian): ongoing small outbreaks globally.
• For weekly influenza updates:
http://www.cdc.gov/flu/weekly
Diagnosis
• Primarily clinical:
cough
,
fever
,
myalgias
, arthralgias, rhinorrhea, pharyngitis (in contrast, viral bronchitis p/w cough ± low-grade temp; usually benign & self-limited) • Respiratory viral panel on nasal washing or sputum/BAL
• Rapid influenza test on nasal swab: Se ~50–70% (? lower for pandemic flu), Sp >95%
• DFA (Se ∼85%), RT-PCR (gold standard) avail. for influenza (PCR distinguishes type)
Treatment
(
NEJM
2008;359:2579)
• Seasonal influenza: treat with neuraminidase inhib. (oseltamivir, zanamivir), which are effective vs. A & B, but resistance emerging. M2 inhib. (amantadine, rimantadine) not recommended due to widespread resistance (
MMWR
2011;60:1).
• Pandemic H1N1: nearly 100% sens. to
oseltamivir
. H5N1: Uncertain resistance pattern.
H7N9: newly emerging in Asia (
NEJM
2013;368:1888)
• Oseltamivir dosed 75 mg PO bid × 5 d. Must start w/in 48h of sx for low-risk; for critically ill or immunosupp., start ASAP even if >48 h.
• Consider inhaled ribavirin for RSV in immunosupp. (eg, BMT, lung tx); limited adult data
Prevention
• Inactivated
influenza vaccine
: incl. H1N1. Rec for
all
>6 mo of age and esp. if pregnant, >50 y, immunosupp., or HCW (
MMWR
2012;61:613) • Isolation, droplet precautions for inPts strongly recommended
• Prophylaxis for high-risk contacts of confirmed influenza: oseltamivir 75 mg PO daily × 10 d
FUNGAL INFECTIONS
Candida
species
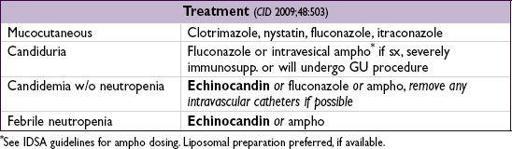
•
Microbiology
: normal GI flora;
C. albicans
& nonalbicans spp. (consider azole resistance if h/o Rx or nonalbicans;
C. parapsilosis
↑ echinocandin resistant). Sensi testing available.
•
Risk factors
: neutropenia, immunosupp., broad-spectrum abx, intravascular catheters (esp. if TPN), IVDU, abd surgery, DM, renal failure, age >65
•
Clinical manifestations
Mucocutaneous: cutaneous (eg, red, macerated lesions in intertriginous zones); oral thrush (exudative, erythematous or atrophic; if unexplained, r/o HIV); esophageal (odynophagia; ± oral thrush); vulvovaginal, balanitis
Candiduria: typically colonization due to broad-spectrum abx and/or indwelling catheter
Candidemia (#4 cause of health care assoc. bloodstream infxn): r/o retinal involvement (req ↑ Rx); endocarditis rare but serious (esp. w/ nonalbicans & prosthetic valve)
Hepatosplenic: intestinal seeding of portal & venous circulation; esp. in acute leukemia
Hematogenous dissemination: lung, brain, meninges,
etc.
Cryptococcus
(
CID
2010;50:291)
•
Epidemiology
: immunosupp. (esp. AIDS) most susceptible; can occur in healthy host, esp. elderly, EtOH, DM. If from Pacific NW, consider
C. gatti
(↑ mortality in healthy host).
•
Clinical manifestations
CNS
(meningitis): HA, fever, meningismus, ↑ ICP, CN abnl, ± stupor, often subacute. Dx: CSF CrAg, India ink stain, fungal cx. Cell counts vary; serum CrAg >1:8 Se/Sp in AIDS.
Other sites: pulm, GU, cutaneous, CNS cryptococcoma.
With any crypto dx, LP all Pts
.
•
Treatment
CNS: If ↑ ICP, repeat large-volume LPs or temp. lumbar drain; few require VP shunt
In HIVor immunosupp. Pts, CNS Rx has induction (ampho ± flucytosine), consolidation and maintenance (fluconazole) phases (
NEJM
2013
;
368:1291). If r/o CNS disease, then fluconazole. Dosing and duration vary by host.
Non-CNS disease in healthy Pts: fluconazole vs. observation, based on clinical setting
Histoplasmosis
(
CID
2007;45;807)
•
Endemic
: central & SE U.S. (esp. in areas w/ bird & bat droppings), river banks elsewhere •
Clinical manifestations
Acute: often subclinical, but may see mild to severe PNA ± cavitary & hilar LAN
Chronic pulm: ↑ productive cough, wt loss, night sweats, apical infiltrates, cavitation
Disseminated (typically in immunosupp.): fever, wt loss, HSM, LAN, oral ulcers, skin lesion, fibrosing mediastinitis, reactive arthritis, pericarditis
•
Treatment
: itraconazole (monitor levels); ampho ± steroids if severe or immunosupp.
Coccidioidomycosis (
CID
2005;41:1217)
•
Endemic
: SW U.S. (San Joaquin or “Valley” fever) •
Clinical manifestations
Acute: 50–67% subclinical; PNA w/ cough, chest pain, fever, arthralgias,
fatigue
Chronic pulm: nodule(s), cavity or progressive fibrocavitary PNA (can be asx or sx)
Disseminated (typically in immunosupp.): fever, malaise, diffuse pulmonary process, bone, skin, & meningeal involvement
Other books
The Slightly Bruised Glory of Cedar B. Hartley by Martine Murray
Flirting With Fame (Flirting With Fame) by Samantha Joyce
What's So Great About America by Dinesh D'Souza
Slipstream by Elizabeth Jane Howard
NEVER FALL FOR THE FORBIDDEN (NEVER FALL SERIES) by Shortridge, Jennifer
The Perfect Hope by Nora Roberts
Werewolf Academy Book 4: Taken by Cheree Alsop
Hatred by Willard Gaylin
Starting Over by Tony Parsons