Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (84 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
9.72Mb size Format: txt, pdf, ePub
Up to 75% of purulent skin/soft tissue infxns, depending on local epi (rapidly increasing)
Clinically indistinguishable from MSSA, often assoc. w/ purulent drainage or exudate
High-risk groups: athletes, military, prison, MSM, communities w/ high prevalence
Often TMP-SMX sensitive; variably clindamycin sensitive (may falsely appear susceptible on lab testing, requires confirmation w/ D-test;
NEJM
2007;357:380)
• Erythema, edema, warmth, pain (rubor, tumor, calor, dolor) • Lymphangitis (proximal red streaking) and regional lymphadenopathy •
Toxic shock syndrome
can occur w/ staph or strep infxn. Fever, HA, N/V, diarrhea, myalgias, pharyngitis, diffuse rash w/ desquamation, HoTN, shock. BCx may be.
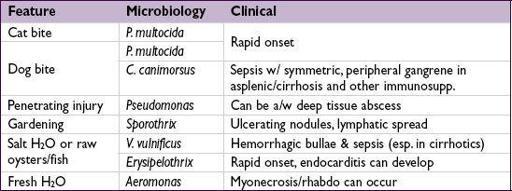
• Bites: skin and oral flora (incl anaerobes) + special exposures:
Diagnosis
• Largely clinical diagnosis; BCx low yield (Se <5% in simple cellulitis) but useful if
• Aspirate of bulla or pus from furuncle or pustule may provide microbiologic dx
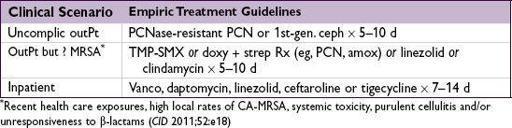
Treatment
•
Limb elevation
; erythema may
worsen
after starting abx b/c bacterial killing → inflam.
• I&D if abscess is present in addition to cellulitis • Worse outcomes if vasc. insuff., edema, immunosupp., resistant orgs. or deeper infxn • In obese Pts, adequate drug dosing important to avoid treatment failure (
J Infect
2012;2:128)
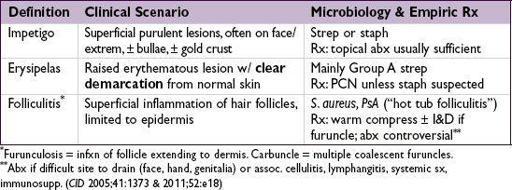
OTHER CUTANEOUS INFECTIONS
“DIABETIC FOOT” = INFECTED NEUROPATHIC FOOT ULCER
Leading cause of DM-related hosp. days & nontrauma amputations
Microbiology
•
Mild
(superficial, no bone or joint involvement): usually
S. aureus
or aerobic streptococci •
Limb-or life-threatening
= deep, bone/joint involvement, systemic tox., limb ischemia • Mono-or polymicrobial with aerobes + anaerobes
aerobes =
S. aureus
, strep, enterococci and GNR (including
Pseudomonas
)
anaerobes = anaerobic streptococci,
Bacteroides
,
Clostridium
(rare)
Clinical manifestations
• Clinical dx: ≥2 classic s/s of inflammation (erythema, warmth, tenderness [may be absent in neuropathy], pain or induration) or purulent secretions ± crepitus (indicating gas and ∴ mixed infection w/ GNR & anaerobes or
Clostridium
) • Complications: osteomyelitis, systemic toxicity (fever, chills, leukocytosis, hyperglycemia)
Diagnostic studies
• Avoid superficial swabs (
only
helpful iffor
S. aureus
and suspect infxn);
wound cx
(eg, deep tissue sample or curettage at ulcer base after débridement) has ↑ Se • Blood cx should be obtained in all Pts,in 10–15%
•
Osteomyelitis should always be ruled out
: probe to bone test for all open wounds in a diabetic foot (high Sp but low Se); imaging (see below);
bone biopsy
best
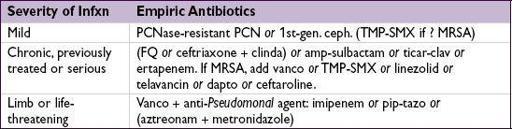
Treatment
(
CID
2012;54:e132)
• Elevation, non–weight-bearing status,
wound care
, glycemic control,
antibiotics
• Evaluation and treatment for venous insufficiency and arterial ischemia •
Many require surgery
: early, aggressive and repeated débridement; revascularization or amputation may be necessary • Management by multidisciplinary team improves outcomes (
Circulation
2006;113:e463)
NECROTIZING FASCIITIS
Definition
• Infection and necrosis of superficial fascia, subcutaneous fat and deep fascia (necrosis of arteries and nerves in subcutaneous fat → gangrene) • Fournier’s gangrene: necrotizing fasciitis of the male genitalia or female perineum
Epidemiology
• Affects healthy individuals but ↑ risk: DM, PVD, EtOH abuse, IDU, immunosupp., cirrhosis
Microbiology
• Type I (after abd/perineal surgery or trauma; in DM, PVD): polymicrobial (w/ anaerobes) • Type II (usually extremities):
Strep pyogenes
±
CA-MRSA
, often healthy w/o obvious portal of entry; up to
1
/
2
have toxic shock syndrome (TSS)
Clinical manifestations
• Need
high degree of clinical suspicion
because of nonspecific physical exam • Most common sites: extremities, abdominal wall and perineum, but can occur anywhere •
Cellulitic skin
D
s
with poorly defined margins +
rapid spread + systemic toxicity
•
Pain out of proportion
to apparent cellulitis; skin hyperesthetic and later anesthetic •
Bullae, darkening of skin to bluish-gray ± crepitus
or radiographically visible gas
Diagnostic signs
• Clinical dx sufficient to initiate
urgent surgical exploration
• Aspiration of necrotic center; BCx; Gram stain; ✓ CK for tissue necrosis
• Imaging:
non-contrast CT
, but do not delay therapy (
Arch Surg
2010;145:452) • Microbiologic dx from Gram stain and culture of surgical specimens
Treatment
• Definitive treatment is
surgical débridement
of necrotic tissue and fasciotomy • Type I: breadth of GNR coverage determined by host, prev hosp, prev Rx and initial
Other books
Calamity in Kent, A British Library Crime Classic by John Rowland
Fixer by Gene Doucette
Vexxed (JUST BREATHE Ephemera Book 4) by Kendall Grey
The Sword Song of Bjarni Sigurdson by Rosemary Sutcliff
To Rescue a Rogue by Jo Beverley
Where did your heart go? (The Heart Trilogy Book 1) by Audrina Lane
The Blushing Bounder (An Iron Seas Short Novella) by Brook, Meljean
Box by John Locke
Brat by Alicia Michaels
Never Love a Stranger by Harold Robbins