Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (40 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

•
Inflammatory bowel disease
• Radiation enteritis, ischemic colitis, neoplasia (colon cancer, lymphoma)
Secretory
(nocturnal diarrhea freq described, no Δ diarrhea after NPO, normal osmotic gap)
•
Hormonal
: VIP (VIPoma, Verner-Morrison), serotonin (carcinoid), thyroxine, calcitonin (medullary cancer of the thyroid), gastrin (Zollinger-Ellison), glucagon, substance P
•
Laxative abuse
• Neoplasm: carcinoma, lymphoma, villous adenoma • ↓ bile acids absorption (s/p ileal resection, Crohn’s) → colonic exposure & ↑ secretion • Lymphocytic colitis, collagenous colitis (may be a/w meds, including NSAIDs)
Motility
(normal osmotic gap)
•
Irritable bowel syndrome
(10–15% of adults;
BMJ
2012;345:e5836;
NEJM
2012;367:1626)
Due to altered intestinal motility/secretion in response to luminal or environmental stimuli w/ enhanced pain perception and dysregulation of the brain–gut axis
Rome III criteria: recurrent abd pain ≥3 d/mo over last 3 mo
plus
≥2 of following: (i) improvement w/ defecation, (ii) onset w/ Δ freq of stool, (iii) onset w/ Δ in form of stool
Rx sx-guided (
AJG
2009;104:51)
Pain
: antispasmodics, TCA, SSRI
Bloating
: rifaximin (
NEJM
2011;364:22), probiotics
Diarrhea
: loperamide, alosetron (5-HT
3
antagonist) for women (↑ risk of ischemic colitis), rifaximin
Constipation
: ↑ fiber 25 g/d, lubiprostone (Cl
–
channel activator)
• Scleroderma; diabetic autonomic neuropathy; hyperthyroidism; amyloidosis; s/p vagotomy
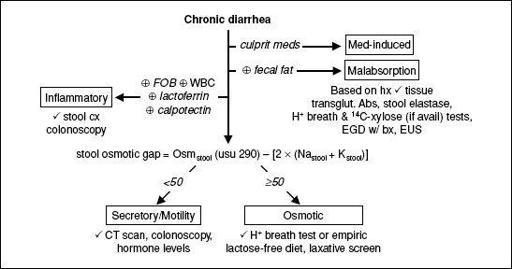
Figure 3-2
Workup of chronic diarrhea
CONSTIPATION & ADYNAMIC ILEUS
Constipation
(
Gastro
2013;144:211 & 218)
•
Definition
(Rome III): ≥2 of the following during last 3 mo at least 25% of time: straining, lumpy/hard stools, incomplete evacuation, sensation of anorectal obstruction, manual maneuvers to facilitate defecation, stool frequency <3 per wk •
Etiology
Functional: normal transit, slow transit, pelvic floor dysfunction, constipation-predom IBS
Meds: opioids, anticholinergics (TCAs & antipsychotics), Fe, CCB, diuretics, NSAIDs
Obstruction: cancer, stricture, rectocele, anal stenosis, extrinsic compression
Metabolic/endo: DM, hypothyroid, uremia, preg, panhypopit, porphyria, ↑ Ca, ↓ K, ↓ Mg
Neuro: Parkinson’s, Hirschsprung’s, amyloid, MS, spinal injury, autonomic neuropathy
•
Diagnosis
: H&P w/ DRE. Labs: consider CBC, electrolytes w/ Ca, TSH
Colonoscopy if alarm sx: wt loss,FOBT, fever, FHx of IBD or colon cancer. Sigmoidoscopy if no alarm sx & <50 y
For functional constipation: Sitzmark study, anorectal manometry, defecography
•
Treatment
: Bulk laxatives (fiber ~20 g/d) → osmotic laxative → stimulant laxative
Bulk laxatives (psyllium, methylcellulose, polycarbophil): ↑ colonic residue, ↑ peristalsis
Osmotic laxatives (Mg, sodium phosphate [avoid if CKD], lactulose): ↑ water in colon
Stimulant laxatives (senna, castor oil, bisacodyl, docusate sodium): ↑ motility & secretion
Enema/suppository (phosphate, mineral oil, tap water, soapsuds, bisacodyl)
Lubiprostone (see “IBS”). Methylnaltrexone and alvimopan for opioid-induced (
AJG
2011;106:835)
Linaclotide ↑ stool freq, ↓ straining/bloating (
NEJM
2011;365;6:527)
Acute pseudo-obstruction (adynamic ileus)
• Definition: loss of intestinal peristalsis in absence of mechanical obstruction
Ogilvie’s = acute colonic adynamic ileus in presence of competent ileocecal valve
• Precipitants: intra-abd process (surgery, pancreatitis, peritonitis); severe medical illness
(eg, PNA, sepsis); intestinal ischemia; meds (opiates, anticholinergics); electrolyte abnl
• Clinical manifestations: abd discomfort, N/V, hiccups, abd distention, ↓ or absent bowel
sounds, no peritoneal signs (unless perforation); cecum ≥10–12 cm → ↑ risk of rupture
• Dx: supine & upright KUB vs. CT→ gas-filled loops of small & large intestine. Must exclude mechanical obstruction (absence of gas in rectum).
• Treatment: NPO, mobilize (walk, roll), d/c Rxs that ↓ intestinal motility, enemas; decompression (NGT, rectal tube, colonoscope); neostigmine (for colonic), methylnaltrexone (for small bowel, ? colonic)
NUTRITION IN HOSPITALIZED PATIENTS
Pathophysiology
• When acutely ill, catabolism > anabolism, carbohydrates preferred due to ↓ fat metab • When recovering, anabolism > catabolism, so body restores protein and muscle loss
Critical illness
(see “Mech Ventilation” for recs in that setting) (
JPEN
2009;33:277)
• Goals not well validated but 18–30 kcal/kg/d & 1.2–1.5g/kg/d protein • Enteral: start w/in 24–48 hrs of admission, trend toward ↓ infxns and mortality in early (<48 h) feeding in critically ill Pts who are adequately nourished at presentation Contraindic: inadequate volume resusc, intestinal obstruction, major GIB, severe vomiting, ischemic bowel • Parenteral: start if unable to tolerate enteral w/in 7 d or evidence of protein/cal malnutrition on admission; may be beneficial in those below calorie goal w/ enteral (
Lancet
2013;381:385) Contraindic: hyperosmolality, severe electrolyte disturbances, severe hyperglycemia; sepsis is
relative
contraindication
End-stage liver disease
(
Clin Gastro & Hep
2012;10:117)
• Nutrition status predicts morbidity/mortality; malnutrition in 50–90% of cirrhotics • Protein requirement
higher
than healthy adults (1–1.5 g/kg/d vs. 0.8 g/kg/d); protein restrict
only
if acute hepatic encephalopathy Supplement vitamins ADEK, zinc, selenium; do not carbohydrate restrict
Refeeding syndrome
(
BMJ
2008;336;1495)
• Fluid/electrolyte shifts in malnourished Pts receiving artificial nutrition; hypophosphatemia is hallmark, but also ↓ K & Mg, hyperglycemia, ↓ thiamine, hypervolemia • Prevention: (1) thiamine 300 mg PO qd, vit B complex tid, MVI; (2) start feeding at ~10 kcal/kg/d (or 25% of estim goal) & ↑ over 3–5 d; advance only when electrolytes are w/in nl range; (3) follow electrolytes and volume status, rehydrating and repleting
DIVERTICULAR DISEASE
DIVERTICULOSIS
Definition & pathobiology
(
Lancet
2004;363:631)
• Acquired herniations of colonic mucosa and submucosa through the colonic wall • Existing dogma is low-fiber diet → ↑ stool transit time and ↓ stool volume → ↑ intraluminal pressure → herniation where vasa recta penetrate, but now ?’d (
Gastro
2012;142:266)
Epidemiology
• Prevalence higher w/ ↑ age (10% if <40 y; 50–66% if >80 y); “Westernized” societies •
Left side
(90%, mostly sigmoid) > right side of colon (except in Asia, where R > L)
Clinical manifestations
• Usually asx, but 5–15% develop diverticular hemorrhage and <5% diverticulitis • Nuts,
etc.
intake in asx diverticulosis does
not
↑ risk of diverticulitis (
JAMA
2008;300:907)
DIVERTICULITIS
Pathophysiology
(
NEJM
2007;357:2057)
• Retention of undigested food and bacteria in diverticulum → fecalith formation → obstruction → compromise of diverticulum’s blood supply, infection, perforation •
Uncomplicated
: microperforation → localized infection •
Complicated
(25%): macroperforation → abscess, peritonitis, fistula (65% w/ bladder), obstruction, stricture
Clinical manifestations
•
LLQ abdominal pain, fever
, nausea, vomiting, constipation • PEx ranges from LLQ tenderness ± palpable mass to peritoneal signs & septic shock • Ddx includes IBD, infectious colitis, PID, tubal pregnancy, cystitis, colorectal cancer
Diagnostic studies
• Plain abdominal radiographs to r/o free air, ileus or obstruction
•
Abdominal CT
(I
+
O
+
): >95% Se & Sp; assess complicated disease (abscess, fistula) • Colonoscopy
contraindicated
acutely ↑ risk of perforation; do 6 wk after to r/o neoplasm
Treatment
(
Am J Gastro
2008;103:1550)
• Mild: outPt Rx indicated if Pt has few comorbidities and can tolerate POs
PO abx: (MNZ + FQ) or amox/clav for 7–10 d; liquid diet until clinical improvement, though recent evidence suggest abx may be unnecessary (
Br J Surg
2012;99:532)
• Severe: inPt Rx if cannot take POs, narcotics needed for pain, or complications
NPO, IV fluids, NGT (if ileus)
IV abx (GNR & anaerobic coverage): amp/gent/MNZ or piperacillin-tazobactam
• Abscesses >4 cm should be drained percutaneously or surgically
• Surgery: if progression despite med Rx, undrainable abscess, free perforation or possibly recurrent disease (≥2 severe episodes) • Colonic stricture: late complication of diverticulitis; Rx w/ endoscopic dilation vs. resection; colonoscopy after 6 wk to exclude neoplasm
Prevention
•
Low-fiber
diet immediately after acute episode;
high-fiber
diet when >6 wk w/o sx • Consider mesalamine ± rifaximin if multiple episodes
• Risk of recurrence 10–30% w/in 10 y of 1st episode; more likely 2nd episode complicated
DIVERTICULAR HEMORRHAGE (ALSO SEE “GASTROINTESTINAL BLEEDING”)
Pathophysiology
• Intimal thickening and medial thinning of vasa recta as they course over dome of diver-ticulum → weakening of vascular wall → arterial rupture • Diverticula more common in left colon; but
bleeding diverticula more often in right colon
Clinical manifestations