Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (18 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
10.07Mb size Format: txt, pdf, ePub
diet: rich in fruits & vegetables, low in saturated & total fat (DASH,
NEJM
2001;344:3)
sodium restriction: ≤2.4 g/d and ideally ≤1.5 g/d (
NEJM
2010;362:2102)
limit alcohol consumption: ≤2 drinks/d in men; ≤1 drink/d in women & lighter-wt Pts
•
Pharmacologic options
(if HTN
or
pre-HTN + diabetes or renal disease)
Pre-HTN
: ARB prevents onset of HTN, no ↓ in clinical events (
NEJM
2006;354:1685)
HTN
:
choice of therapy controversial, concomitant disease and stage may help guide Rx
uncomplicated
: thiazide if likely salt sensitive (eg, elderly, black, obese), o/w start w/ ACEI or CCB (
NEJM
2009;361:2153). bB not first line (
Lancet
2005;366:1545).
+
high-risk CAD
: ACEI or ARB (
NEJM
2008;358:1547); ACEI + CCB superior to ACEI + thiazide (
NEJM
2008;359:2417) or bB + diuretic (
Lancet
2005;366:895)
+
angina
: bB, CCB, nitrates
+
post-MI
: ACEI, bB ± aldosterone antagonist (see “ACS”)
+
HF
: ACEI/ARB, bB, diuretics, aldosterone antagonist (see “Heart Failure”)
+
2
°
stroke prevention
: ACEI (
Lancet
2001;358:1033); ? ARB (
NEJM
2008;359:1225) +
diabetes mellitus
: ACEI or ARB; can also consider diuretic, bB or CCB
+
chronic kidney disease
: ACEI/ARB (
NEJM
1993;329:1456 & 2001;345:851 & 861)
•
Tailoring therapy
if stage 1, start w/ monoRx; if not at goal, Δ to different class rather than adding 2nd agent
if stage 2, consider starting w/ combo (eg, ACEI + CCB;
NEJM
2008;359:2417) as most will require ≥2 drugs; low–mod doses of 2 drugs generally preferred over max dose of 1 drug (b/c of dose-related AEs)
if resistant [= HTN despite ≥3 drugs (incl diuretic) at opt doses], consider noncompliance, volume overload, secondary causes; ? renal artery denervation (
Lancet
2010;376:1903)
•
Secondary causes
Renovascular
: control BP w/ diuretic + ACEI/ARB (watch for ↑ Cr w/ bilat. RAS) or CCB Atherosclerosis risk-factor modification: quit smoking, ↓ chol. If refractory HTN, recurrent flash pulm edema, worse CKD, consider revasc
For atherosclerosis: stenting ↓ restenosis vs. PTA alone, but no clear improvement in BP or renal function vs. med Rx (
NEJM
2009;361:1953;
Annals
2009;150:840)
For FMD (usually more distal lesions): PTA ± bailout stenting
Renal parenchymal disease
: salt and fluid restriction, ± diuretics
Endocrine etiologies
: see “Adrenal Disorders”
•
Pregnancy:
methyldopa, labetalol, nifedipine, hydralazine; avoid diuretics; ACEI/ARB
HYPERTENSIVE CRISES
•
Hypertensive emergency
: ↑ BP → acute target-organ ischemia and damage
neurologic damage: encephalopathy, hemorrhagic or ischemic stroke, papilledema
cardiac damage: ACS, HF/pulmonary edema, aortic dissection
renal damage: proteinuria, hematuria, acute renal failure; scleroderma renal crisis
microangiopathic hemolytic anemia; preeclampsia-eclampsia
•
Hypertensive urgency
: SBP >180 or DBP >120 (?110) w/ min. or no target-organ damage
Precipitants
• Progression of essential HTN ± medical noncompliance (esp. clonidine) or Δ in diet • Progression of renovascular disease; acute glomerulonephritis; scleroderma; preeclampsia • Endocrine: pheochromocytoma, Cushing’s
• Sympathomimetics: cocaine, amphetamines, MAO inhibitors + foods rich in tyramine • Cerebral injury (do
not
treat HTN in acute ischemic stroke unless Pt getting lysed, extreme
BP (>220/120), Ao dissection, active ischemia or HF (
Stroke
2003;34:1056)
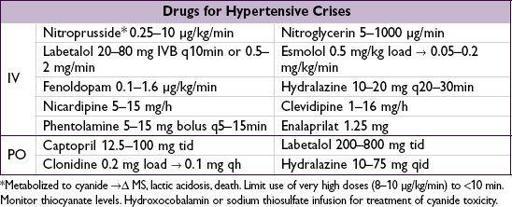
Treatment (
Chest
2007;131:1949)
• Tailor goals to clinical context (eg, more rapid lowering for Ao dissection) • Emergency: ↓ MAP by ~25% in
mins to 2 h
w/ IV agents (may need arterial line for monitoring); goal DBP <110 w/in 2–6 h, as tolerated • Urgency: ↓ BP in
hours
using PO agents; goal normal BP in ~1–2 d • Watch UOP, Cr, mental status: may indicate a lower BP is not tolerated
AORTIC ANEURYSMS
Definitions
•
True
aneurysm (dilation of all 3 layers of aorta) vs.
false
(rupture contained by adventitia) •
Location
: root (annuloaortic ectasia), thoracic aortic aneurysm (TAA), thoracoabdominal aortic aneurysm (TAAA), abdominal aortic aneurysm (AAA) •
Type
: fusiform (circumferential dilation) vs. saccular (localized dilation of aortic wall)
Epidemiology (
Circ
2010;121:e266;
Nat Rev Cardiol
2011;8:92)
• In U.S.,
15,000 deaths/y from aortic ruptures; overall
50,000 deaths/y from Ao disease •
TAA
::
1.7:1;
60% root/ascending Ao; 40% descending Ao; arch & TAAA rarer
Risk factors:
HTN
;
atherosclerosis
; congenital (
bicuspid AoV
, Turner’s);
connective tissue diseases
(Marfan, Ehlers-Danlos type IV, Loeys-Dietz);
aortitis
(Takayasu’s, GCA, spondyloarthritis, IgG4, syphilis); familial syndromes; chronic AoD; trauma
•
AAA
: ~4–8% prev. in those >65 y; 5–10× more common invs.
; mostly infrarenal
Risk factors = similar to
atherosclerosis
:
smoking
, HTN, hyperlipidemia, age, FHx
Pathophysiology (
NEJM
2009;361:1114;
Nat Med
2009;15:649)
•
LaPlace’s law
: tension across a cylinder ∝ [(ΔP × r) / (wall thickness)]
•
TAA
: medial degeneration = muscle apoptosis, elastin fiber weakening, mucoid infiltration •
AAA
: atherosclerosis & inflammation → matrix degeneration → medial weakening • Inflammatory and infectious (“mycotic”) aneurysms relatively rare
Screening (
Annals
2005;142:203;
JAMA
2009;302:2015;
Circ
2010;121:e266)
•
TAA
: no consensus guidelines; ? screen if bicuspid AoV or first-degree relative •
AAA
: ✓ for pulsatile abd mass; U/S>60 y w/ FHx of AAA &
65–75 y w/ prior tobacco
Diagnostic studies (
Circ
2005;111:816 & 2010;121:e266)
Other books
Playing For Keeps by R.L. Mathewson
The Keepers Book Two of the Holding Kate Series by Cole, LaDonna
Mine for a Day by Mary Burchell
Eye on Orion by Laura D. Bastian
Cracker! by Kadohata, Cynthia
Angelborn by Penelope, L.
Menage a Fairy (A Fairy Novel) by Keraleigh, Anna
Olive Oil and White Bread by Georgia Beers
Lizzie Marshall's Wedding by Emily Harvale
Jacks and Queens at the Green Mill by Marie Rutkoski