Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (19 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
10.82Mb size Format: txt, pdf, ePub
•
Contrast CT
: quick, noninvasive, high Se & Sp for all aortic aneurysms •
TTE/TEE
: TTE most useful for root and proximal Ao; TEE can visualize other sites of TAA •
MRI
: preferred over CT for aortic root imaging for TAA; also useful in AAA but time-consuming; noncontrast “black blood” MR to assess aortic wall •
Abdominal U/S
: screening and surveillance test of choice for infrarenal AAA
Treatment (
Circ
2006;113:e463; 2008;177:1883; 2010;121:1544 & e266)
•
Risk factor modification
: smoking cessation, statin to achieve LDL-C <70 mg/dL
•
BP control
: b
B
(↓ dP/dt) ↓ aneurysm growth (
NEJM
1994;330:1335);
ACEI
a/w ↓ risk of rupture (
Lancet
2006;368:659),
ARB
may ↓ rate of aortic root growth in Marfan (
NEJM
2008;358:2787); no burst activity/exercise requiring Valsalva maneuvers (eg, heavy lifting) •
Indications for surgery
: individualize based on FHx, body size, gender
TAA
: sx; asc Ao ≥5.5 cm (? 5.0 cm Marfan, bicuspid AoV; 4.2–4.4 cm Loeys-Dietz); descending >6 cm; ↑ >0.5 cm/y; aneurysm ≥4.5 cm and planned AoV surgery
AAA
: infrarenal ≥5.5 cm (
NEJM
2002;346:1437) but consider ≥5.0 cm in; sx; ↑ >0.5 cm/y; inflam/infxn
•
Endovascular aneurysm repair
(EVAR) (
NEJM
2008;358:494;
Circ
2011;124:2020)
↓ short-term mort., bleeding, LOS; but long-term graft complic. (3–4%/y; endoleak, need for reintervention, rupture) necessitate periodic surveillance, with no proven Δ in overall mortality, except ? in those <70 y (
NEJM
2010;362:1863, 1881 & 2012;367:1988)
Guidelines support open repair or EVAR for infrarenal AAA in good surg candidates
In Pts unfit for surgery or high peri-op risks: ↓ aneurysm-related mortality but no Δ in overall mortality over medical Rx (
NEJM
2010;362:1872). EVAR noninferior (? superior) to open repair in ruptured AAA w/ favorable anatomy (
Ann Surg
2009;250:818).
TEVAR (thoracic EVAR) for descending TAA ≥5.5 cm may ↓ peri-op morbidity, no proven mortality benefit (
Circ
2010;121:2780;
JACC
2010;55:986;
J Thorac CV Surg
2010;140:1001)
Complications (
Circ
2010;121:e266;
Nat Rev Cardiol
2011;8:92)
•
Pain
: gnawing chest, back or abdominal pain; new or worse pain may signal rupture •
Rupture
: risk ↑ w/ diameter,, current smoking, HTN
TAA
: ~2.5%/y if <6 cm vs. 7%/y if >6 cm;
AAA
: ~1%/y if <5 cm vs. 6.5%/y if 5–5.9 cm
rupture p/w severe constant pain and hemorrhagic shock; ~80% mortality at 24 h
•
Acute aortic syndromes
(qv) •
Thromboembolic ischemic events
(eg, to CNS, viscera, extremities) •
Compression of adjacent structures
(eg, SVC, trachea, esophagus, laryngeal nerve)
Follow-up (
Circ
2010;121:e266;
Nat Rev Cardiol
2011;8:92; JAMA 2013;309:806)
• Expansion rate
0.1 cm/y for TAA,
0.3–0.4 cm/y for AAA • AAA: q3y if 3–3.9 cm; q6–12 mo if 4.0–5.4 cm (? q2y if 4–4.4) • TAA: 6 mo after dx to ensure stable, then annually.
• Screen for CAD, PAD and aneurysms elsewhere, esp. popliteal. About 25% of Pts w/
TAA will also have AAA, and 25% of AAA Pts will have a TAA: consider pan-Ao imaging.
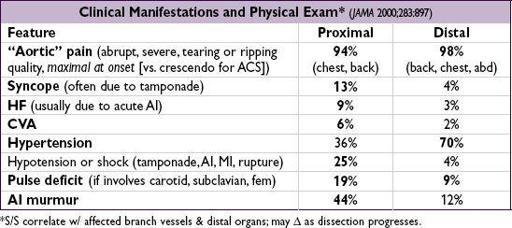
ACUTE AORTIC SYNDROMES
Definitions (
Circ
2003;108:628 & 2010;121:e266;
Eur Heart J
2012;33:26)
•
Aortic dissection
: intimal tear → blood extravasates into Ao media (creates false lumen) •
Intramural hematoma
(IMH): vasa vasorum rupture → medial hemorrhage that does not communicate with aortic lumen; 6% of aortic syndromes; clinically identical to AoD
•
Penetrating ulcer
: atherosclerotic plaque penetrates elastic lamina → medial hemorrhage
Classification (proximal twice as common as distal)
•
Proximal
: involves ascending Ao, regardless of origin (= Stanford A, DeBakey I & II) •
Distal
: involves descending Ao only, distal to L subclavian art. (= Stanford B, DeBakey III)
Risk factors
•
Hypertension
(h/o HTN in >70% of dissections);
male sex
(~70%); cocaine •
Connective tissue disease
:
Marfan
(fibrillin-1): arachnodactyly, joint disloc., pectus, ectopia lentis, MVP;
Ehlers-Danlos
type IV (type III procollagen): translucent skin; bowel or uterine rupture;
Loeys-Dietz
(TGFbR)
;
annuloaortic ectasia, familial AoD; PCKD
•
Congenital aortic anomaly
: bicuspid AoV, coarctation (eg, in Turner’s syndrome) •
Aortitis
(eg, Takayasu’s, GCA, Behçet’s, syphilis, now rare);
pregnancy
(typ. 3rd trim.) •
Trauma
: blunt, deceleration injury; IABP, cardiac or aortic surgery, cardiac catheterization
Diagnostic studies (
Circ
2005;112:3802; & 2010;121:e266;
Annals
2006;166:1350)
• Check bilateral BP and radial pulses for symmetry •
CXR
: abnl in 60–90% (↑ mediastinum, left pl effusion), but
cannot
be used to r/o dissection •
CT
: quick, noninvasive, readily available, Se ≥93% & Sp 98%; however, if& high clin. suspicion → additional studies (
2
⁄
3
w/ AoD have ≥2 studies;
AJC
2002;89:1235) •
TEE
: Se >95% prox, 80% for distal; can assess cors/peric/AI; “blind spot” behind trachea •
MRI
: Se & Sp >98%, but time-consuming test & not readily available •
Aortography
: Se ~90%, time-consuming, cannot detect IMH; can assess branch vessels •
D-dimer
: Se/NPV ~97%; ? <500 ng/mL to r/o dissec (
Circ
2009;119:2702); does not r/o IMH
Treatment (
Lancet
2008;372:55;
Circ
2010;121:1544;
JACC
2013;61:1661)
•
Initial Medical
: ↓
dP/dt
targeting HR ~60 & central BP 100–120 (or lowest that preserves perfusion; r/o pseudohypotension, eg, arm BP ↓ due to subclavian dissection)
first
with IV
b
B
(eg, propranolol, esmolol, labetalol) to blunt reflex ↑ HR & inotropy that would occur in response to vasodilators; verap/dilt if bB contraindic.
then
↓
SBP with IV vasodilators
(eg, nitroprusside)
control pain with MSO
4
prn to blunt sympathetic response
•
Proximal
: surgery (root replacement);
all acute
; chronic if c/b progression, AI or aneurysm •
Distal
: med Rx unless c/b progression, branch artery involvement → malperfusion/ ischemia, refractory HTN, refractory pain, rapid ↑ aneurysm size, rapid ↑ false lumen size. Repeat imaging: routinely (eg, 7 d, 3 wk, then q yr) & with any clinical or significant lab Δ. If complic., endovascular repair (covered stent graft to seal off entry, fenestrate flap, open occluded branch) preferred over surgery due to possible ↓ mort. (
JACC
2013;61:1661).
Other books
Sandpipers' Secrets by Jade Archer
Hunted (Dark Protectors) by Zanetti, Rebecca
A Company of Heroes Book Five: The Space Cadet by Ron Miller
Needing You by Fike, T. Renee
Tales of the Taoist Immortals by Eva Wong
Your Gravity: Part One by L. G. Castillo
Dawn of a New Age: A Sons of Satrina Novel by Kristan Belle
Finding Floyd by Melinda Peters
Buzzard Bay by Bob Ferguson