Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (22 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
2.91Mb size Format: txt, pdf, ePub
Cardioversion
• Consider pharm or electrical cardioversion w/ 1st AF episode or if sx;
if AF >48 h, 2–5% risk stroke w/ cardioversion (
pharmacologic or electric
) ∴ either TEE to r/o thrombus or ensure therapeutic anticoagulation for ≥3 wk prior • Likelihood of success ∝ AF duration & atrial size; control precip. (eg, vol status, thyroid) • Consider pre-Rx w/ antiarrhythmic drugs (esp. if 1st cardioversion attempt fails) • For pharmacologic cardioversion, class III and IC drugs have best proven efficacy • If SR returns (spont. or w/ Rx), atria may be
mech. stunned
; also, high risk of recurrent AF over next 3 mo. ∴
Anticoag postcardioversion
≥
4–12 wk
(? unless <48 h and low risk).
Nonpharmacologic therapy
•
Radiofrequency ablation
(circumferential pulm. vein isolation;
Lancet
2012;380:1509): ~80% success; reasonable alternative to AAD in sx persistent or paroxysmal AF w/o ↑↑ LA or ↓ EF (NEJM 2012;367:1587; RAAFT 2, HRS 2012) • Surgical “maze” procedure (70–95% success rate) option if undergoing cardiac surgery • LA appendage closure/resection: reasonable if another indication for cardiac surgery
percutaneous closure noninferior to warfarin, ↓ risk of ICH, but w/ procedural complic; additional studies & approaches underway (Lancet 2009;374:534; PREVAIL, ACC 2013)
Oral anticoagulation (Chest 2012;141:e531S; EHJ 2012;33:2719; Circ 2013;127:1916)
•
All valvular AF
as stroke risk very high • Nonvalvular AF: stroke risk ~4.5%/y; anticoag → 68% ↓ stroke; use a risk score to guide Rx:
CHADS
2
: CHF
(1 point),
HTN
(1), Age ≥75 y (1), DM (1), prior Stroke/TIA (2)
CHA
2
DS
2
-
VASc
: adds 65–74 y (1), >75 y (2); vasc dis. (1);sex (1)
score
>
2
→
anticoag; score 1
→
consider anticoag
or ASA (? latter reasonable if risk factor 65–74 y, vasc dis. or); antithrombotic Rx even if rhythm cntl
•
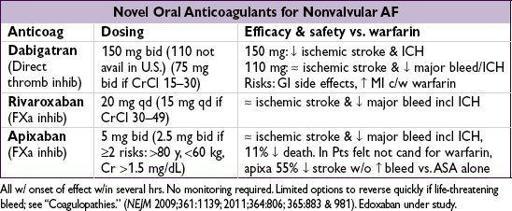
Rx options
:
factor Xa or direct thrombin inhib
(nonvalv only; no monitoring required) or
warfarin
(INR 2–3; w/ UFH bridge if high risk of stroke); if Pt refuses anticoag, consider
ASA + clopi or, even less effective, ASA alone (NEJM 2009;360:2066)
SYNCOPE
Definition
• Symptom of sudden transient loss of consciousness due to global cerebral hypoperfusion • If CPR or cardioversion required, then SCD and not syncope (different prognosis)
Etiologies
(
NEJM
2002;347:878;
JACC
2006;47:473;
Eur Heart
J
2009;30:2631)
•
Neurocardiogenic
(a.k.a. vasovagal, ~20%;
NEJM
2005;352:1004): ↑ sympathetic tone → vigorous contraction of LV → mechanoreceptors in LV trigger ↑ vagal tone (hyperactive Bezold-Jarisch reflex) → ↓ HR (cardioinhibitory) and/or ↓ BP (vasodepressor)
cough, deglutition, defecation, & micturition → ↑ vagal tone and thus can be precipitants
related disorder: carotid sinus hypersensitivity (exagg vagal resp to carotid massage) •
Orthostatic hypotension
(10%)
hypovolemia/diuretics, deconditioning; vasodilat. (esp. if combined w/chronotropes)
autonomic neuropathy [1° = Parkinson’s, Shy-Drager, Lewy body dementia, POTS (dysautonomia in the young); 2° = DM, EtOH, amyloidosis, CKD] (
NEJM
2008;358:615)
•
Cardiovascular
Arrhythmia
(15%)
Bradyarrhythmias: SSS, high-grade AV block,chronotropes, PPM malfunction
Tachyarrhythmias: VT, SVT (syncope rare unless structural heart disease or WPW)
Mechanical
(5%)
Endocardial/Valvular: AS, MS, PS, prosthetic valve thrombosis, myxoma
Myocardial: pump dysfxn from MI or outflow obstruction from HCMP (but usually VT)
Pericardial: tamponade
Vascular: PE, PHT, aortic dissection, ruptured AAA, subclavian steal
•
Neurologic
(10%): seizure (technically not syncope), TIA/CVA, vertebrobasilar
insufficiency, dissection of cerebral arteries, migraine, narcolepsy
• Misc. causes of LOC (but not syncope): hypoglycemia, hypoxia, anemia, psychogenic
Workup
(etiology cannot be determined in
~40% of cases)
•
H&P incl. orthostatic VS have highest yield and most cost effective
(
Archives
2009;169:1299) •
History
(from Pt and
witnesses
if available)
activity and posture before the incident
precipitating factors: exertion (AS, HCMP, PHT), positional Δ (orthostatic hypotension), stressors such as sight of blood, pain, emotional distress, fatigue, prolonged standing, warm environment, N/V, cough/micturition/defecation/swallowing (neurocardiogenic), head turning or shaving (carotid sinus hypersens.); arm exercise (subclavian steal)
prodrome (eg, diaphoresis, nausea, blurry vision): cardiac <~5 sec, vasovagal >~5 sec
associated sx: chest pain, palp., neurologic, postictal, bowel or bladder incontinence (convulsive activity for <10 sec may occur w/ transient cerebral HoTN & mimic seizure)
•
PMH
: prior syncope, previous cardiac or neurologic dis.; no CV disease at baseline → 5% cardiac, 25% vasovagal; CV disease → 20% cardiac, 10% vasovagal (
NEJM
2002;347:878) •
Medications that may act as precipitants
vasodilators: a-blockers, nitrates, ACEI/ARB, CCB, hydralazine, phenothiazines, antidep.
diuretics;chronotropes (eg, bB and CCB)
proarrhythmic or QT prolonging: class IA, IC or III antiarrhythmics (see “ECG”)
psychoactive drugs: antipsychotics, TCA, barbiturates, benzodiazepines, EtOH
•
Family history
: CMP, SCD, syncope (vasovagal may have genetic component) •
Physical exam
VS including
orthostatics
(if supine → standing results in >20 mmHg ↓ SBP, >10 mmHg ↓ DBP, or >10–20 bpm ↑ HR), BP in both arms
Other books
Gavin's Submissives by Sam Crescent
I So Don't Do Famous by Barrie Summy
Cast in Stone by G. M. Ford
Dusky Duke and the Gypsy Pirate Princess by Kya Lind
Captured by her Alien Guard by Elsa Silk
The Road to Omaha by Robert Ludlum
Mastered By Love by Tori Minard
Discovering Pleasure by Marie Haynes
Taste of Tenderloin by Gene O'Neill
Flashes of Me by Cynthia Sax