Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (81 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

• Unknown source: continue antibiotics until afebrile
and
ANC >500 cells/µL
• Less clear when to d/c abx when Pt is afebrile but prolonged neutropenia
Role of hematopoietic growth factors
(
NEJM
2013;368:1131)
• Granulocyte (G-CSF) and granulocyte-macrophage (GM-CSF) colony-stimulating factors can be used as 1° prophylaxis when expected FN incidence >20% or as 2° prophylaxis after FN has occurred in a previous cycle (to maintain dose-intensity for curable tumors). CSFs ↓ rate of FN but have not been shown to impact mortality.
• Colony-stimulating factors can be considered as adjuvant therapy in high-risk FN Pts
SPINAL CORD COMPRESSION
Clinical manifestations
(
Lancet Neuro
2008;7:459)
• Metastases located in vertebral body extend and cause epidural spinal cord compression •
Prostate
,
breast
and
lung
cancers are the most common causes, followed by renal cell
carcinoma, NHL and myeloma
•
Site of involvement
:
thoracic
(60%), lumbar (25%), cervical (15%) • Signs and symptoms:
pain
(>95%,
precedes neuro
D
s
),
weakness
,
autonomic dysfunction
(urinary retention, ↓ anal sphincter tone),
sensory loss
Diagnostic evaluation
• Always take back pain in Pts with solid tumors very seriously • Do
not
wait for neurologic signs to develop before initiating evaluation b/c duration & severity of neurologic dysfunction before Rx are best predictors of neurologic outcome • Urgent
whole-spine MRI
(Se 93%, Sp 97%); CT myelogram if unable to get MRI
Treatment
•
Dexamethasone
(10 mg IV × 1 stat, then 4 mg IV or PO q6h)
initiate immediately
while awaiting imaging if back pain + neurologic deficits
• Emergent RT or surgical decompression if confirmed compression/neuro deficits • Surgery + RT superior to RT alone for neuro recovery in solid tumors (
Lancet
2005;366:643) • If pathologic fracture causing compression → surgery; if not surgical candidate → RT
TUMOR LYSIS SYNDROME
Clinical manifestations
(
NEJM
2011;364:1844;
BJH
2010;149:578)
• Large tumor burden or a rapidly proliferating tumor → spontaneous or chemotherapy-induced release of intracellular electrolytes and nucleic acids • Most common w/ Rx of high-grade lymphomas (
Burkitt’s
) and leukemias (
ALL
,
AML
,
CML in blast crisis
); rare with solid tumors; rarely due to spontaneous necrosis • Electrolyte abnormalities: ↑ K, ↑ uric acid, ↑ PO
4
→ ↓ Ca •
Renal failure
(urate nephropathy)
Prophylaxis
• Allopurinol 300 mg qd to bid PO or 200–400 mg/m
2
IV (adjusted for renal fxn) & aggressive hydration prior to beginning chemotherapy or RT
• Rasburicase (recombinant urate oxidase) 0.15 mg/kg or 6 mg fixed dose (except in obese Pts) & aggressive hydration prior to beginning chemotherapy or RT (see below)
Treatment
•
Avoid
IV contrast and NSAIDs • Allopurinol + aggressive IV hydration ± diuretics to ↑ UOP
• Consider alkalinization of urine w/ isotonic NaHCO
3
to ↑ UA solubility & ↓ risk of urate nephropathy (controversial: may cause metabolic alkalosis or Ca
3
(PO4)
2
precipitation) • Rasburicase (0.1–0.2 mg/kg × 1, repeat as indicated) for ↑↑ UA, esp. in aggressive malig; UA level must be drawn on ice to quench
ex vivo
enzyme activity (
JCO
2003;21:4402;
Acta Haematol
2006;115:35). Avoid in G6PD deficiency as results in hemolytic anemia.
• Treat hyperkalemia, hyperphosphatemia and symptomatic hypocalcemia • Hemodialysis may be necessary; early renal consultation for Pts w/ renal insuffic. or ARF
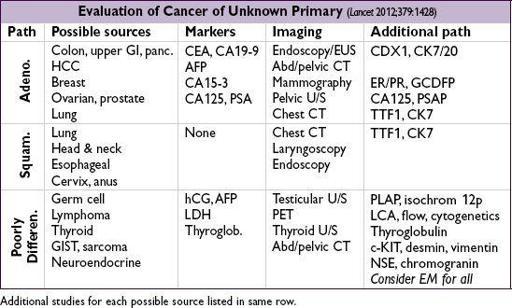
CANCER OF UNKNOWN PRIMARY SITE
• Bony mets: common primary tumors include breast, lung, thyroid, kidney, prostate
NOTES
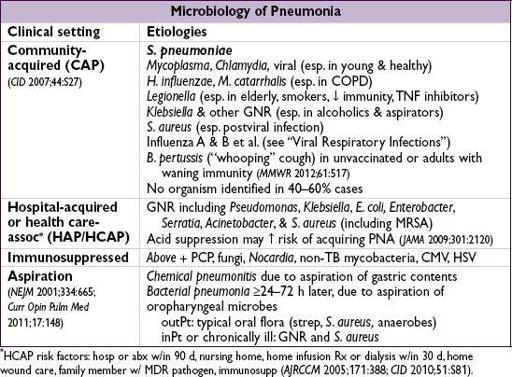
PNEUMONIA
Clinical manifestations
• “Typical”: acute onset of fever, cough w/ purulent sputum, dyspnea, consolidation on CXR
• “Atypical” (originally described as cx): insidious onset of dry cough, extrapulm sx (N/V, diarrhea, headache, myalgias, sore throat), patchy interstitial pattern on CXR
• S/s & imaging do
not
reliably distinguish between “typical” (
S. pneumo
,
H. flu
) and “atypical” (
Mycoplasma
,
Chlamydia, Legionella
, viral); ↑ aminotransferases & ↓ Na w/
Legionella
Diagnostic studies
•
Sputum Gram stain
: utility debated. Good sample (ie, sputum not spit) has <10 squamous cells/lpf. Purulent sample has >25 PMNs/lpf.
•
Sputum bacterial culture
: transport to lab w/in 1–2 h of collection • Blood cultures (
before antibiotics!
):in ~10% of inPts, depending on pathogen •
CXR
(PA & lateral; see Radiology inserts) → tap effusions if >5 cm or severe PNA • Other:
S
a
O
2
or P
a
O
2
, arterial pH (if severe), CBC w/ diff, Chem-20; HIV test (if unknown) • Other micro based on clinical suspicion (paired serologies available for most atypicals):
Mycoplasma
: PCR of throat or sputum/BAL
before
first dose abx
Legionella
urinary Ag (detects
L. pneumophila
L1 serotype, 60–70% of clinical disease)
S. pneumoniae
urinary Ag (Se 50–80%, Sp >90%)
MTb: induced sputum for AFB stain and mycobacterial cx (
empiric respiratory isolation while pending
); avoid quinolones if suspect TB; request rapid DNA probe if stain
Induced sputum for PCP if HIVor known ↓ cell-mediated immunity
• Viral testing (DFA or PCR) on nasopharyngeal swab or sputum; rarely viral cx • Bronchoscopy: consider if immunosupp., critically ill, failing to respond, or chronic pneumonia. Also if suspected TB or PCP, but inadequate orsputum cx. Some pathogens need specific cx (eg,
Legionella
on BCYE); collaborate with lab.