Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (85 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
10.98Mb size Format: txt, pdf, ePub
Gram stain; eg, carbapenem or (3rd-gen ceph + amp + [clinda or metronidazole])
• Type II: PCN + clinda. If ↑ risk of CA-MRSA, + vanco. If concern for strep, IVIG.
Prognosis
• Generally fatal if untreated; reported mortality 20–50%
CLOSTRIDIAL MYONECROSIS (GAS GANGRENE)
Definition
• Life-threatening, fulminant clostridial infection of skeletal muscle •
Wound contamination
w/ clostridial spores after
trauma
(penetrating or crush injury) • Most commonly
C. perfringens
;
C. septicum
assoc w/ cancer (GI, heme), even w/o trauma
Clinical manifestations
• Incubation period 6 h to 2–3 d • Sense of heaviness/pain, often at site of trauma; rapid worsening; marked systemic toxicity • Bronze skin discoloration, tense bullae, serosanguineous or dark fluid and necrotic areas •
Crepitus
present but not prominent (gas is in muscle), may be obscured by edema
Diagnostic studies
• Gram stain:
lg
,
Grambacilli w/ blunt ends
(can be Gram-variable)
, few polys • Bacteremia in ~15%
• Plain radiographs: gas dissecting into muscle
Treatment
•
Surgical exploration with débridement
, fasciotomies and amputation if necessary •
Antibiotics
: high-dose
penicillin G
24 MU IV divided q2–3h +
clinda
900 mg IV q8h
OSTEOMYELITIS
Infection of bone due to hematogenous seeding or direct spread from contiguous focus
Microbiology
(
NEJM
1997;336:999;
Lancet
2004;364:369)
•
Hematogenous
:
S. aureus
; mycobacterial infection of vertebral body = Pott’s disease •
Contiguous focus
(may be acute or chronic)
open fracture, orthopedic surgery, etc.:
S. aureus
and
S. epi
skin breakdown + vasc. insuffic. (eg, diabetic foot):
polymicrobial
(aerobic + anaerobic GPC & GNR)
Clinical manifestations
• Surrounding soft-tissue compromise ± fistula to superficial skin • ± Fever, malaise and night sweats (more common in hematogenous than contiguous) • Vertebral osteomyelitis (seen in Pts >50 y): unremitting, focal back pain, usually fever (
NEJM
2010;362:1022)
Diagnostic studies
(
JAMA
2008;299:806)
• Identification of the causative organism is key •
Culture from tissue
(surgical sampling/needle bx),
not
swabs of ulcers or fistulae drainage • High suspicion in diabetic foot (see above) if can probe ulcer to bone or ulcer >2 cm
2
•
Blood cultures
(more oftenwith acute hematogenous osteomyelitis) •
ESR
>70 greatly increases likelihood of osteo (
JAMA
2008;299:806) • Imaging
Plain radiographs: normal early in disease; lytic lesions seen after 2–6 wk
MRI
: can detect very early changes (overall Se 90%, Sp 82%;
Archives
2007;167:125)
CT: can demonstrate periosteal reaction and cortical and medullary destruction
CT & MRI very Se but ↓ Sp; falseif contig focus w/ periosteal reaction, Charcot Ds
Radionuclide imaging: very Se but non-Sp (falseif soft tissue inflammation)
Treatment
•
Antibiotics
(based on cx data) × 4–8 wk •
Surgery
should be considered for any of the following: acute osteo that fails to respond to medical Rx, chronic osteo, complications of pyogenic vertebral osteo (eg, early signs of cord compression, spinal instability, epidural abscess) or infected prosthesis
EPIDURAL ABSCESS
Etiology
• Hematogenous spread (
2
/
3
): skin infection, soft tissue (dental abscess) or endocarditis • Direct extension (
1
/
3
): vertebral osteo, sacral ulcer, spinal anesthesia or surgery, LP
• Risk factors: diabetes, renal failure, alcoholism, IVDU, immunosupp.
•
S. aureus
most common pathogen, increasing incidence of MRSA
Clinical manifestations
•
Back pain
(unremitting including midline) + often
fever
± nerve root or cord signs
Diagnostic studies
•
MRI
• Aspiration of abscess fluid for Gram stain & cx or operative Gram stain & cx • Blood cx (frequently)
Treatment
•
Antibiotics ± surgery
(decompressive laminectomy and débridement) for failure to improve on medical Rx or early s/s of cord compression (w/ vertebral osteo and epidural abscess, may see paraplegia 48–72 h after first signs)
INFECTIONS OF THE NERVOUS SYSTEM
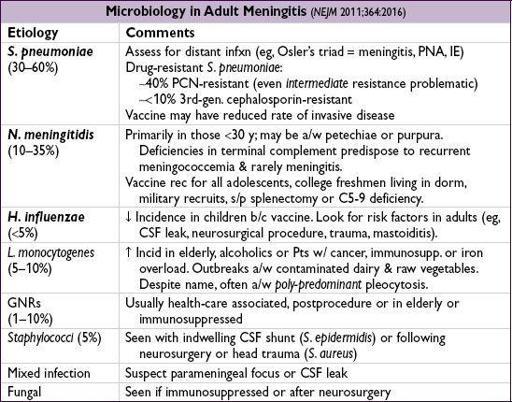
ACUTE BACTERIAL MENINGITIS
Definition
• Bacterial infection of the subarachnoid space
Clinical manifestations
(
NEJM
2006;354:44;
Lancet
2012;380:1684)
•
Fever
(77%),
headache
(87%),
stiff neck
(31%),
photosensitivity
, Δ
MS
(69%) (defined as GCS <14),
seizures
(5%); 2 of 4 (fever, HA, stiff neck, Δ MS) present in 95%
• Presentation may be
atypical
(eg, lethargy w/o fever) in elderly and immunosupp.
Physical exam
•
Nuchal rigidity
(Se 31%),
Kernig’s sign
(Pt supine, hip flexed at 90°, knee flexed at 90°;if passive extension of knee results in resistance),
Brudzinski’s sign
(Pt supine and limbs supine;if passive neck flexion → involuntary hip and/or knee flexion)
Other books
The Rancher's First Love by Brenda Minton
Steppenwolf by Hermann Hesse, David Horrocks, Hermann Hesse, David Horrocks
For Love and Honor by Cathy Maxwell, Lynne Hinton, Candis Terry
Marie Harte - [PowerUp! 08] by Killer Thoughts
The Whale Caller by Zakes Mda
Fallout by James W. Huston
The Courts of Love: The Story of Eleanor of Aquitaine by Jean Plaidy
B009RYSCAU EBOK by Bagwell, Gillian
Carolina Home by Virginia Kantra
Sullivans Island-Lowcountry 1 by Dorothea Benton Frank