Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (88 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
3.69Mb size Format: txt, pdf, ePub
•
Adjust abx regimen & duration
based on valve (NVE vs. PVE); if possible, de-escalate abx to organism-directed Rx guided by
in vitro
sensi's or local patterns of Rx-resist. Add rifampin for PVE due to staph spp. (usually after BCxto ↓ risk resistance develops).
• Repeat BCx qd until Pt defervesces and BCx; usually 2–3 d • Fever may persist even >1 wk after appropriate abx or due to metastatic sites • Systemic anticoagulation relatively
contraindicated
given risk of hemorrhage in cerebral embolic strokes; w/o stroke, can continue short-acting anticoag for pre-existing indication • Monitor for complications of endocarditis (CHF, conduction block, new emboli, etc., which can occur even on abx) and of abx Rx (interstitial nephritis, ARF, neutropenia, etc.) • Duration of Rx: usually
4–6 wk
. With NVE & sx <3 mo → 4 wk of abx; sx >3 mo → ≥6 wk. Uncomplicated right-sided NVE or PCN-S strep spp → 2 wk may be comparable.
• Posthospitalization outPt IV abx monitoring; future endocarditis Ppx
Indications for surgery
(
EHJ
2009;30:2369;
Circ
2010;121:1005 & 1141)
• Several days of abx (if possible) to ↓ recurrence of infection and improve structural integrity of tissue to receive prosthesis •
Severe valvular dysfunction
→
refractory CHF
:
emergent
if refractory cardiogenic shock (ie, despite ICU-level Rx);
urgent
(w/in days) if persistent refractory heart failure;
elective
(w/in wks) if asx severe AI or MR
•
Uncontrolled infxn
(urgent surgery w/in days): periannular abscess (10–40% NVE, 60– 100% PVE), fistula, worsening conduction, PVE w/ dehiscence, ↑ veg. size or persistent sepsis (eg,BCx [? or fever] after ~1 wk of appropriate IV abx and no drainable metastatic focus or other identifiable cause) •
Organism
: consider surgery for
S. aureus
, fungal or multiRx resistant organisms •
Systemic embolism
(20–50%): risk 4.8/1000 Pt days in 1st wk, 1.7/1000 thereafter
urgent surgery if L-sided w/ >10 mm veg & severe AI/MR (
NEJM
2012;366:2466) or if recurrent emboli, embolism & >10 mm veg, or >15 mm veg despite approp. abx
cerebral emboli
no longer considered contraindic to surgery unless hemorrhage (then ideally wait 1 mo) or severe stroke (
Stroke
2006;37:2094)
•
PVE
: esp. w/ valve dysfxn
or
dehiscence
or S. aureus
or GNR infection. Seek ID eval.
Prognosis
• NVE: non-IVDU
S. aureus
→ 30–45% mortality; IVDU
S. aureus
(typically right-sided) → 10–15% mortality; SBE → 10–15% mortality • PVE → 23% mortality • Aortic valve worse prognosis than mitral valve
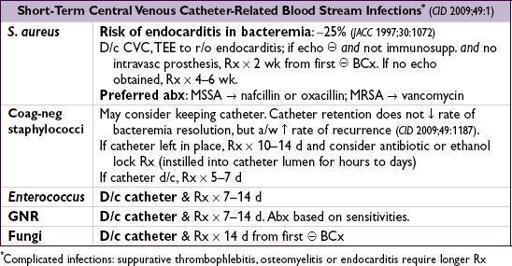
BACTEREMIA
Etiologies
• 1° infxn due to direct inoculation of the blood, frequently assoc w/ intravascular catheters. Catheter-related bloodstream infection = same org from peripheral cx
and
cath tip cx
or
cx drawn from catheter (
CID
2009;49:1).
• 2° infxn due to infection in another site (eg, UTI, lung, biliary tree, skin) spreading to blood
Microbiology
• 1° infxn/indwelling catheters (
ICHE
2008;29:996): coag-neg staph (incl
S. epi
and others) 34%,
S. aureus
10%, enterococci 16%,
Candida
spp. 12%,
Klebsiella
spp. 5%
• 2° infxn: dependent on source
Risk factors for true bacteremia
(
JAMA
2012;308:502)
•
Pt
: fever, shaking chills, IVDU, comorbidities, immunosupp, indwelling catheter, SIRS
•
Organism
more likely pathogenic:
S. aureus
, b-hemolytic strep, enterococci, GNR,
S. pneumo, Neisseria
less likely pathogenic: coag-neg staph (~10%), diphtheroids,
Propionibacterium
(~0%)
•
Time to growth
: <24 h → higher risk, >72 h → lower risk (except for slow-growing organisms such as HACEK group) •
Factors increasing the likelihood of endocarditis
: high-grade bacteremia w/o source, persisting after line removal or drainage of focal source, in hosts at risk for endocarditis or w/ organisms known to cause IE (Duke criteria); emboli
Diagnosis
•
Blood Cx
: prior to 1st abx dose if possible; 10 cc in each Cx bottle; add’l Cx if high risk
Treatment
•
1
°
infxn
: antibiotics based on Gram stain/culture results; tailor abx to sensitivities empiric therapy for GPC: vanco to cover coag-neg staph and MRSA while awaiting sensi
•
2
°
infxn
: assess for primary source of infection and treat. Source control essential for cure and to prevent recurrence.
•
PersistentlyBCx
: d/c indwelling catheters, consider metastatic infxn, infected thrombosis or infected prosthetic material (joint, abscess, vascular graft, pacemaker, etc.)
TUBERCULOSIS
Epidemiology
• U.S.: 10–15 million infected (10× ↑ risk if foreign-born or minority); worldwide: ~2 billion • After resurgence in U.S. 1984–1992, rates declined, though slower than CDC goals • Multidrug resistant (
MDR
)
TB:
resistant to isoniazid (INH) and rifampin (RIF). Can occur as new (not previously treated) infxn if exposed in former Soviet Republics, Russia, China • Extensively drug resistant
(XDR) TB
resistant to INH, RIF, FQ and injectables •
Pts more likely to develop TB disease
(
NEJM
2011;364:1441)
High-prevalence populations
(more likely to be exposed to & infected): immigrant from high-prevalence area, homeless, IDU or medically underserved, resident or worker in jail or long-term facility, HCW at facility w/ TB, close contact to Pt w/ active TB
High-risk populations
(infected & likely to progress to active disease): HIV, immunosupp. incl. biologics, uncontrolled DM & smoking, close contact w/ active TB Pt, underweight, CKD, organ Tx, IVU, EtOH, malnourished, cancer, gastrectomy
Other books
This is Not a Novel by David Markson
Emma Who Saved My Life by Wilton Barnhardt
The Fire Within (The Last Dragon Chro) by Chris D'Lacey
Vanquish by Pam Godwin
The State by Anthony de Jasay by Jasay, Anthony de
Choke by Diana López
Houseboat Days: Poems by John Ashbery
The Lonely Girl by Wilson, Gracie
Shadowed by Sin by Layna Pimentel
An Enigmatic Disappearance by Roderic Jeffries