Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (114 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
4.48Mb size Format: txt, pdf, ePub
biopsy → microgranulomas, fibrinoid necrosis and thrombosis of small arteries and
veins with eosinophilic infiltrates
• Treatment: high-dose
corticosteroids
+ cyclophosphamide if severe
Renal-limited vasculitis
• Small vessel pauci-immune vasculitis causing RPGN w/o other organ involvement • Dx studies: 80%ANCA (MPO > PR3); biopsy with pauci-immune GN ± granulomas • Treatment identical to that for GPA/MPA
IMMUNE COMPLEX–ASSOCIATED SMALL-VESSEL VASCULITIS
Henoch-Schönlein purpura (HSP)
•
IgA-mediated
vasculitis w/ predilection for
skin
,
GI tract
and
kidneys
• Epidemiology:>
, children > adults, onset in winter > summer • May develop after upper respiratory tract infection (esp. strep) or drug exposure • Clinical manifestations
palpable purpura
on extensor surfaces (lower extremity first) & buttocks
polyarthralgias
(nondeforming) esp. involving hips, knees, & ankles
colicky
abdominal pain
± GIB or intussusception
nephritis ranging from
microscopic hematuria
& proteinuria to ESRD
• Dx studies:
skin bx w/ immunofluorescence
→
leukocytoclastic vasculitis
w/
IgA
and
C3
deposition in vessel wall; renal bx → mesangial IgA deposition
• Treatment: often self-limiting over 4 wk; steroids ± DMARDs for renal or severe disease
Cryoglobulinemic vasculitis (see “Cryoglobulinemia”)
Connective tissue disease–associated vasculitis
• Small vessel vasculitis a/w
RA
,
SLE
or
Sjögren’s syndrome
• Clinical manifestations
distal arteritis: digital ischemia, livedo reticularis, palpable purpura, cutaneous ulceration
visceral arteritis: pericarditis and mesenteric ischemia
peripheral neuropathy
• Dx studies: skin/sural nerve bx, angiography, EMG; ↓ C′ in SLE;RF or anti-CCP in RA • Treatment: steroids, cyclophosphamide, MTX (other DMARDs)
Cutaneous leukocytoclastic angiitis
• Heterogeneous group of clinical syndromes due to
immune complex deposition
in capillaries, venules and arterioles; includes
hypersensitivity vasculitis
• Overall the most common type of vasculitis • Etiologies
drugs: PCN, ASA, amphetamines, levamisole, thiazides, chemicals, immunizations
infections: Strep, Staph, endocarditis, TB, hepatitis
malignancy (paraneoplastic)
• Clinical manifestations: abrupt onset of
palpable purpura
and
transient arthralgias
after exposure to the offending agent; visceral involvement rare but can be severe • Dx studies: ↑ ESR, ↓ complement levels, eosinophilia; ✓ U/A;
skin biopsy
→ leukocytoclastic vasculitis
w/o
IgA deposition
in skin (to distinguish from HSP); if etiology not clear, consider ANCA, cryoglobulins, hepatitis serologies, ANA, RF
• Treatment: withdrawal of offending agent ± rapid prednisone taper
Behçet’s syndrome
(
Curr Rheum Opin
2010;12:429)
•
Systemic vasculitis
affecting all vessel sizes, a/w
oral and/or genital ulcers
• Epidemiology: usually young adults (25–35 y); a/w HLA-B51 in areas of highest prevalence on the old Silk Road (Turkey, Middle East and other Asian countries) • Classification criteria (#1 + ≥2 others is 91% Se & 96% Sp; Lancet 1990;335:1078) 1. recurrent
oral aphthous ulceration
(≥3× in 1 y, usually 1st manifestation) 2. recurrent
genital ulceration
(labia in females, scrotum in males) 3.
eye
lesions: uveitis, scleritis, retinal vasculitis, optic neuritis (may threaten vision) 4.
skin
lesions: pustules, papules, folliculitis, erythema nodosum (scarring) 5.pathergy test (prick forearm w/sterile needle → pustule) (not sensitive in Caucasians) • Other clinical manifestations: most recur but are not chronic
arthritis: mild, ± symmetric, nondestructive, involving knees and ankles
neurologic: usually involvement of midbrain parenchyma; peripheral neuropathy rare
vascular: superficial or deep vein thrombosis (25%); arterial stenosis, occlusion and aneurysm can also occur; low incidence of thromboembolism
• Dx studies: ↑ ESR/CRP; ulcer swab to r/o HSV; ulcer bx nonspecific; ophtho eval if sx • Treatment (Rheumatology 2007;46:736; Ann Rheum Dis 2008;67:1656 & 2009;68:1528)
mucocutaneous
mild:
topical steroids
,
colchicine
(esp. for erythema nodosum), dapsone
severe: oral steroids, steroid-sparing agents
arthritis: NSAIDs, colchicine, steroids, steroid-sparing agents
ocular:
topical and/or systemic steroids
± steroid-sparing agents
steroid-sparing: AZA, anti-TNF, CYC (large vessel and CNS ds), CsA, MTX, IFNɑ-2A
venous thrombosis: steroids and anticoagulation (careful if aneurysm present)
IGG4-RELATED DISEASE
Definition & etiology
(
NEJM 2012;366:539)
• Responsible for
tumor-like inflammatory lesions
of nearly every organ/tissue • Etiology unclear: ? autoimmune; unclear role of IgG4 Ab; may have h/o atopy
Clinical manifestations
• Commonly pancreatitis, aortitis, cholangitis, sialadenitis, orbital structures, retroperitoneal fibrosis • Multiple lesions may be present synchronously or metachronously
Diagnosis
(Mod Pathol 2012;25:1181)
•
Biopsy
w/ specific histopathology & immunohistochemistry findings: lymphoplasmacytic infiltrate w/ significant IgG4+ plasma cell infiltrate, fibrosis, obliterative phlebitis • ↑ serum IgG4 in 40%; not specific seen in GPA, bronchiectasis, etc (Modern Rheum 2012;22:419)
Treatment
•
Prednisone
vs. rituximab (Medicine 2012;91:57)
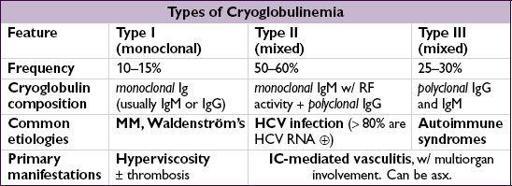
CRYOGLOBULINEMIA
Definition & types
(Lancet 2012;379:348)
•
Proteins that precipitate on exposure to the cold and redissolve on rewarming
, characterized by their composition •
Cryoglobulins
=proteins that precipitate from serum and plasma when cooled • Distinguish from cryo
fibrinogenemia
=proteins (eg, fibrin, fibrinogen) that precipitate only from plasma; found in autoimmune dis, malignancies, infxns; unclear clinical significance
Other books
Double Play at Short by Matt Christopher
Cursed by Chemistry by Kacey Mark
Trouble Under the Tree (A Nina Quinn Mystery) by Heather Webber
Yes, Justin by Michele Zurlo
Rebel's Consort - Phoenix Book 1 by KH LeMoyne
Happily Ever Afterlife by Nikki Hoff
Almost Heaven by Jillian Hart
Day 9 by Robert T. Jeschonek
With This Fling... by Kelly Hunter
The Invasion of Adam (Tork and Adam Book 2) by Claire Davis, Al Stewart