Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (115 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
7.46Mb size Format: txt, pdf, ePub
Etiologies
• Infections (types II & III): viral (
HCV
, HBV, HIV, HAV, EBV, CMV), bacterial (endocarditis, strep, etc.), fungal (coccidiomycosis, etc.) and parasitic (malaria, amoebiasis) • Hematologic diseases
type I: MM, CLL, Waldenström’s
type II: B-cell lymphomas, solid organ malignancies
• Autoimmune syndromes (type III > II):
Sjögren’s syndrome
, SLE, RA, PAN
• Essential (idiopathic) in 10% of cases
• Renal transplant recipients (Clin Nephrol 2008;69:239)
Pathophysiology
• Chronic immune stimulation and/or lymphoproliferation → cryoglobulin generation • Type I: cryo precipitation in microcirculation →
hyperviscosity
&
vascular occlusion
• Types II/III: defective/insufficient immune complex (IC) clearance → IC-mediated inflammation of blood vessels w/ complement activation →
vasculitis
Clinical manifestations
(systemic sx usually due to type II
> III)
• Most patients with cryoglobulinemia are asx
• Type I: hyperviscosity (cold worsens sx) → H/A, visual disturbance, livedo, digital ischemia • Type II: vasculitis (sx not affected by cold exposure)
General:
weakness
, low-grade fever
Dermatologic (54–80%): lower extremity
purpura
, livedo reticularis, leg ulcers
Joint (44–70%): symmetric, migratory
arthralgias
of small or medium joints
Renal (50%):
glomerulonephritis
(proteinuria, hematuria, ARF, HTN, edema)
Neurologic (17–60%):
peripheral neuropathy
(polyneuropathy > mononeuritis multiplex)
Hematologic: anemia, thrombocytopenia, ↑ risk of B-cell lymphoma
GI (5%): abdominal pain, hepatosplenomegaly, abnormal LFTs
Diagnostic studies
• ✓ Cryoglobulins; must keep blood warmed to 37°C at all times en route to lab; early cooling causes falsecryoglobulin, loss of RF and ↓↓ complement • Cryocrit is quantification of cryoprotein, does not always correlate w/ disease activity • False ↑ in WBC or plt on automated CBC, due to cryoprecipitation
• Type I: ✓ serum viscosity, symptomatic if ≥4.0 centipoise; complement levels normal • Type II: ↓
C4 levels
, variable C3 levels, ↑ ESR,rheumatoid factor (RF) ✓
HCV, HBV, & HIV serologies
in all Pts w/ mixed cryoglobulinemia Bx of affected tissue: hyaline thrombi; vasculitis w/ mixed inflammatory infiltrates of small vessels; leukocytoclastic vasculitis in purpuric lesions
Treatment
(Autoimmun Rev 2011;10:444; Arth Rheum 2012;64:604; Blood 2012;119:5996)
•
Treat underlying disorder
:
Lymphoproliferative disease: chemotherapy and/or radiation
HCV: antivirals ± immunosuppression for severe disease
Connective tissue-related disease: DMARD/steroids ± rituximab
• Type I: Plasma exchange if hyperviscosity
• Type II: NSAIDs for control of mild symptoms for Pts w/ normal renal function
Rituximab or cyclophosphamide for major organ involvement
Plasmapheresis or plasma exchange in severe, life-threatening disease
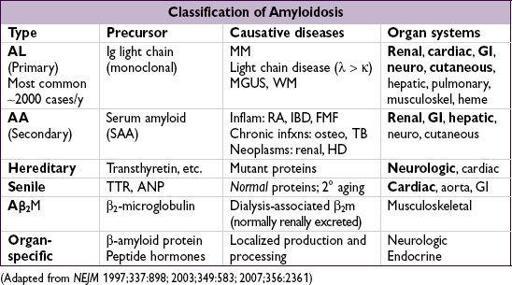
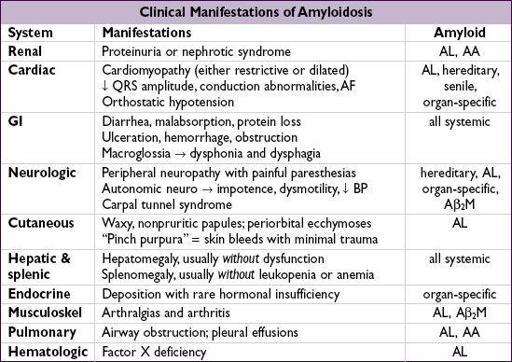
AMYLOIDOSIS
The deposition of misfolded and insoluble fibrous proteins in normal organs and tissues.
Diagnostic studies
• If suspect AL → ✓ SIEP & UIEP (↑ Se vs. SPEP & UPEP) & free light chains, ± BM bx • If suspect renal involvement ✓ U/A (proteinuria)
• If suspect cardiac involvement: ✓ ECG (↓ voltage, conduction abnl), echo (biventricular thickening with “granular sparkling” appearance; ↑ wall w/o ↑ volt 75% Se, 95% Sp), MRI • Biopsy (abdominal SC fat pad, rectal or affected tissue) → apple-green birefringence on
Congo red stain
; fat pad bx Se 60–85%, Sp 90–100%
• Genetic testing for hereditary forms
Treatment
• AL: ? high-dose melphalan → auto HSCT if limited organ dysfxn (NEJM 2007;357:1083); o/w low-dose melphalan + dexamethasone; novel agents (eg, bortezomib, lenalidomide, thalidomide) being evaluated (J Hematol Oncol 2011;4:47) • AA: Rx underlying disease; colchicine for FMF esp. to prevent progressive renal disease (NEJM 2007;356:23); eprodisate promising for renal disease (NEJM 2007;356:2349) • For hereditary amyloidoses in which amyloid precursor protein is produced by the
liver (eg, TTR), liver transplantation may prevent further deposition
• Cardiac involv.: diuretics; avoid dig & CCB; avoid vasodilators; ? ICD for 1° prevention • Heart, kidney and liver Tx may be considered in those w/ advanced disease
Prognosis
• AL amyloid: median survival ~12–18 mo; if cardiac involvement, median survival ~6 mo • AA amyloid: median survival ~11 y (NEJM 2007;356:2361)
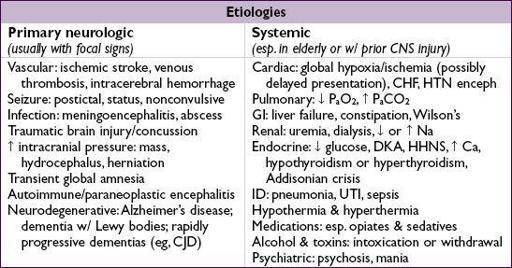
CHANGE IN MENTAL STATUS
Definitions (description of patient & timing is most helpful)
•
Unresponsive
: implies ↓ arousal or ability to follow commands, specify w/ exam
•
Delirium
(aka acute confusional state or encephalopathy): acute change in attention and consciousness with fluctuations. May include sleep–wake dysregulation, autonomic changes, abnormal sensory perception and changes in affect as additional features.
•
Dementia:
impaired cognition, often incl. memory. Usually chronic & progressive, eventually encompassing more anatomical & functional parts of the nervous system.
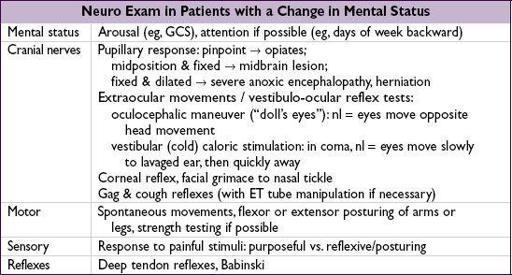
Initial evaluation
•
History
(witness & background
crucial
): time course, previous illnesses including dementia or psych; head trauma; meds, drug/alcohol use; infection/immune status
•
General physical exam
:
vital signs
, signs of trauma, asterixis, stigmata of liver disease, embolic phenomena, signs of drug use, nuchal rigidity (may be present in meningitis or SAH, but
do not test
if possible trauma/cervical spine fracture)
•
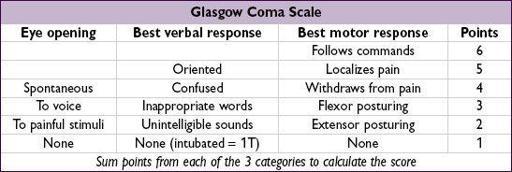
Neurologic exam
(most meaningful off sedatives/paralytics): look for focality or s/s of ↑ ICP (eg, HA, vomiting, papilledema, unilateral dilated pupil, ↑ BP)
Other books
Trio by Robert Pinget
Punished! by David Lubar
Breastfeeding My Boss - An Erotic Story (Lactating Sex) by Lynn Mixon
Winter's Dawn by Moon, Kele
Watersmeet by Ellen Jensen Abbott
Enter the Bad Boy (Sweet Surrender) by Coolomon, Matt
Controlled: The Dollhouse, Part Two by Stacia Stone
Lady Sophie's Christmas Wish by Grace Burrowes
Son of Serge Bastarde by John Dummer
Butterfly Winter by W.P. Kinsella