Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (78 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
2.06Mb size Format: txt, pdf, ePub
•
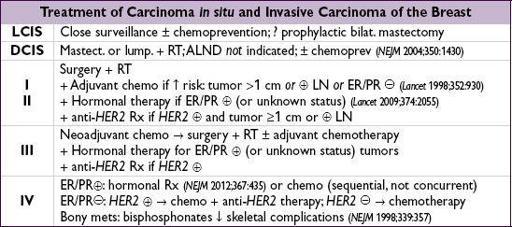
Systemic therapy:
for stage I-III except tumors <1 cm (complex risk assessment needed).
http://www.adjuvantonline.com/index.jsp
can guide use of chemo and/or hormonal Rx.
Chemotherapy
(
Lancet
2008;371:29): in neoadjuvant setting usually
anthracycline
-based (eg,
a
driamycin +
c
yclophosphamide). Sequential Rx w/
taxane
(eg, paclitaxel) → small ↑ survival (
NEJM
2007;357:1496; 2010;362:2053 & 2010;363:2200).
Anti-HER2 therapy
(growing list of agents) in
HER2tumors (
NEJM
2012;366:176)
trastuzumab
(Herceptin; anti-
HER2
mAb) ↑ survival (
NEJM
2001;344:783); give after anthracycline or w/ taxane to avoid cardiotox (
JCO
2002;20:125 &
NEJM
2011;365:1273) lapatinib (tyrosine kinase inhib. of
HER2
&
EGFR
) + trastuzumab ↑ survival after failing trastuzumab (
JCO
2012;30:2585); dual inhib. initial Rx ↑ response (
Lancet
2012;379:633) pertuzumab (anti-
HER2
mAb, prevents dimerization) ↑ progression-free survival when added to trastuzumab as first-line Rx for metastatic dis. (
NEJM
2012;366:109) trastuzumab emtansine (T-DM1,
HER2
mAb conjugated to microtubule inhibitor) ↑ survival compared to second-line lapatinib + capecitabine (
NEJM
2012;367:1783)
Bevacizumab
(anti-VEGF): ? in neoadjuvant Rx if
HER2(
NEJM
2012;366:299 & 310)
Hormonal (in ER/PRor unknown status)
tamoxifen
: 39% ↓ recurrence and 30% ↓ breast cancer mortality in pre-and postmenopausal patients; 10 y of Rx superior to 5 y (
Lancet
2011;378:771 & 2013;381:805)
aromatase inhibitors (AI)
(anastrozole, letrozole, exemestane): ~18% ↓ recurrence vs. tamoxifen in
postmenopausal
Pts (
Lancet
2005;365:60;
NEJM
2005;353:2747)
everolimus ↑ progression-free survival if postmenopausal & failed AI (
NEJM
2012;366:520)
2nd-line: ovarian ablation with LHRH agonists (goserelin) or oophorectomy if
premenopausal
; pure antiestrogens (fulvestrant) if
postmenopausal
Prevention
(with selective estrogen receptor modulator [SERM] or AI)
• Tamoxifen: ↓ risk contralat. breast CA as adjuvant Rx. Approved for 1° prevent. if ↑ risk: ↓ invasive breast ca, but ↑ DVT & uterine CA; ? ↑ in mortality (
Lancet
2002;360:817 ).
• Raloxifene: ↓ risk of invasive breast cancer & vertebral fx, ↑ risk of stroke & DVT/PE (
NEJM
2006;355:125);tamoxifen in prevention of breast cancer w/ ↓ risk of DVT/PE & cataracts, trend toward ↓ uterine cancer (
JAMA
2006;295:2727 ) • Exemestane in high-risk postmenopausal ↓ invasive breast ca by 65% (
NEJM
2011;364:2381) •
BRCA1/2: intensified surveillance as described above. Prophylactic bilat. mastectomy → ~90% ↓ risk; bilat. salpingo-oophorectomy ↓ risk of ovarian
and
breast cancer.
PROSTATE CANCER
Epidemiology and risk factors
(
NEJM
2003;349:366)
• Most common cancer in U.S. men; 2nd most common cause of cancer death in men • Lifetime risk of prostate cancer dx
16%; lifetime risk of dying of prostate cancer
3%
• More common with ↑ age (rare if <45 y), in African Americans and ifFHx • ↑ risk w/
BRCA2
(4.7) and
BRCA1
(1.8) (
JNCI
1999;91:1310 & 2002;94:1358)
Clinical manifestations
(usually asymptomatic at presentation)
•
Obstructive sx
(more common with BPH): hesitancy, ↓ stream, retention, nocturia •
Irritative sx
(also seen with prostatitis): frequency, dysuria, urgency • Periprostatic spread: hematuria, hematospermia, new-onset erectile dysfunction • Metastatic disease: bone pain, spinal cord compression, cytopenias
Screening
(
NEJM
2012;367:e11)
•
Digital rectal exam
(DRE): size, consistency, lesions •
PSA:
4 ng/mL cut point neither Se nor Sp; can ↑ with BPH, prostatitis, acute retention, after bx or TURP, and ejaculation (
no significant
↑
after DRE, cystoscopy
); 15% of men >62 y w/ PSA <4 & nl DRE have bx-proven T1 cancer (
NEJM
2004;350:2239) • Per American Cancer Soc. men ≥50 y (or ≥ 45 y if African-Am orFHx) should discuss PSA screening w/ their MD; USPSTF rec. against screening in asx males (no reduction in prostate cancer-related mortality) (
NEJM
2009;360:1310;
Annals
2012;157:120)
Diagnostic and staging evaluation
•
Transrectal ultrasound
(TRUS)
guided biopsy
, with 6–12 core specimens •
Histology
:
Gleason grade
(2–10; low grade ≤6) = sum of the differentiation score (1 = best, 5 = worst) of the 2 most prevalent patterns in the bx; correlates with prognosis •
Imaging
: to evaluate extraprostatic spread bone scan: for PSA >10 ng/mL, high Gleason grade or clinically advanced tumor abdomen-pelvis CT: inaccurate for detecting extracapsular spread and lymph node mets endorectal coil MRI: improves assessment of extracapsular spread
Other books
A Muse for Mishka (Wiccan-Were-Bear #12) by R.E. Butler
L.A. Fire by Bailey, Sarah
Reunion with Her Alpha (Paranormal Werewolf Shifter Romance) by Wilson, Joanna
Catch My Breath by M. J. O'Shea
Going Platinum, by Helen Perelman
Djinn by Laura Catherine
What Happens At Christmas by Victoria Alexander
The Jewel Box by C Michelle McCarty
Promises to Keep by Ann Tatlock
Highland Wolf (Highland Brides) by Greiman, Lois