Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (17 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
7.01Mb size Format: txt, pdf, ePub
if RA pressure remains elevated after drainage, may have effusive-constrictive disease (
NEJM
2004;350:469) or myocardial dysfxn (eg, from concomitant myocarditis)
Treatment
• Volume (but be careful as overfilling can worsen tamponade) andinotropes (avoid bB) • Avoid vasoconstrictors as will ↓ stroke volume & potentially ↓ HR
•
Pericardiocentesis
(except if due to aortic or myocardial rupture, in which case
consider removing just enough fluid to reverse PEA en route to emergent surgery)
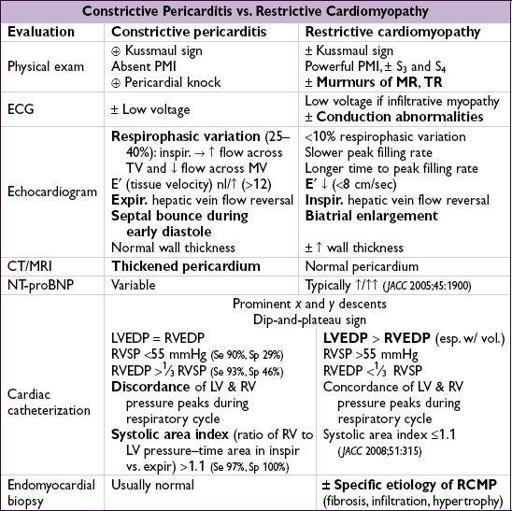
CONSTRICTIVE PERICARDITIS
Etiology (
Circ
2011;124:1270)
• Any cause of pericarditis (~1–2% incidence overall after acute pericarditis) • Highest risk w/
TB
,
bacterial
,
neoplastic
, connective tissue, postcardiac surgery •
Viral/idiopathic
, as most common cause of pericarditis, also account for signif proportion
Pathophysiology
• Adhesion of visceral and parietal pericardial layers → rigid pericardium that limits diastolic filling of ventricles → ↑ systemic venous pressures • Venous return is limited only after early rapid filling phase; ∴ rapid ↓ in RA pressure with atrial relaxation and opening of tricuspid valve and
prominent x and y descents
• Kussmaul sign: JVP does not decrease with inspiration (↑ venous return with inspiration but negative intrathoracic pressure not transmitted to heart because of rigid pericardium)
Clinical manifestations (
NEJM
2011;364:1350)
• Right-sided > left-sided heart failure (systemic congestion > pulmonary congestion)
Physical exam
• ↑
JVP
with
prominent y descent
,Kussmaul sign
(Ddx: tricuspid stenosis, acute cor pulmonale, RV failure and RV infarct, RCMP) • Hepatosplenomegaly, ascites, peripheral edema. Consider on Ddx of idiopathic cirrhosis.
• PMI usually not palpable,
pericardial knock
, usually no pulsus paradoxus
Diagnostic studies
• ECG: nonspecific, AF common (up to 33%) in advanced cases • CXR: calcification (MTb most common), esp. in lateral view (although not specific) • Echocardiogram: ± thickened pericardium, “
septal bounce
” = abrupt displacement of septum during rapid filling in early diastole • Cardiac catheterization
atria:
Ms
or
Ws
(prominent
x
and
y
descents)
ventricles:
dip-and-plateau
or
square-root sign
(rapid ↓ pressure at onset of diastole, rapid ↑ to early plateau)
discordance
between LV & RV pressure peaks during respiratory cycle (
Circ
1996;93:2007)
• CT or
MRI
: thickened pericardium (>4 mm; Se ~80%), w/ tethering (
Circ
2011;123:e418)
Treatment
• Diuresis for intravascular volume overload; surgical pericardiectomy in advanced cases • ? MRI able to predict reversibility with anti-inflammatory agents (
Circ
2011;124:1830)
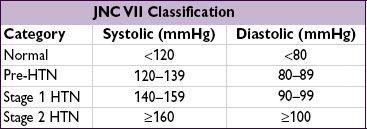
HYPERTENSION
BP should be determined by making ≥2 measurements separated by >2 min. Confirm stage 1 w/in 2 mo; can Rx stage 2 immediately.
Epidemiology (
JAMA
2003;290:199 & 2010;303:2043)
• Prevalence 30% in U.S. adults; >68 million affected (29% in whites, 33.5% in blacks) • Only 50% of patients with dx of HTN have adequate BP control
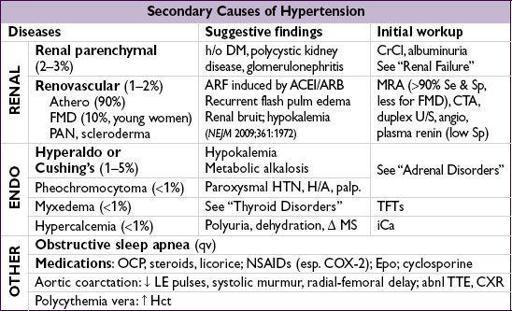
Etiologies
•
Essential
(95%): onset 25–55 y;FHx. Unclear mechanism but ? additive microvasc
renal injury over time w/ contribution of hyperactive sympathetics (
NEJM
2002;346:913).
↑ Age → ↓ arterial compliance → syst HTN. Genetics also involved (
Nat
ure 2011;478:103).
•
Secondary
: Consider if Pt <20 or >50 y or if sudden onset, severe, refractory HTN
Standard workup
• Goals: (1) identify CV risk factors or other diseases that would modify prognosis or Rx;
(2) reveal 2° causes of hypertension; (3) assess for target-organ damage
• History: CAD, HF, TIA/CVA, PAD, DM, renal insufficiency, sleep apnea, preeclampsia;FHx for HTN; diet, Na intake, smoking, alcohol, prescription and OTC meds, OCP
• Physical exam: ✓
BP in both arms
; funduscopic exam, cardiac (LVH, murmurs), vascular (bruits, radial-femoral delay), abdominal (masses or bruits), neuro exam • Testing: K, BUN, Cr, Ca, glc, Hct, U/A, lipids, TSH, urinary albumin:creatinine (if ↑ Cr, DM, peripheral edema), ? renin, ECG (for LVH), CXR, TTE (eval for valve abnl, LVH)
Complications of HTN
•
Each
↑
20 mmHg SBP or
10 mmHg DBP
→
2
× ↑
CV complications
(
Lancet
2002;360:1903) • Neurologic:
TIA/CVA
, ruptured aneurysms, vascular dementia • Retinopathy: stage I = arteriolar narrowing; II = copper-wiring, AV nicking; III = hemorrhages and exudates; IV = papilledema • Cardiac:
CAD
,
LVH
,
HF, AF
• Vascular: aortic dissection, aortic aneurysm (HTN = key risk factor for aneurysms) • Renal: proteinuria,
renal failure
Treatment (
Lancet
2012;380:591)
• Goal: <140/90 mmHg; if DM or CKD goal is <130/80 mmHg (nb, in DM, target of <120 does not ↓ CV risk & ↑ adverse events;
NEJM
2010;362:1575) •
Treatment results in 50%
↓
HF, 40%
↓
stroke, 20–25%
↓
MI
(
Lancet
2000;356:1955); benefits of Rx’ing stage II HTN extend to Pts >80 y, goal BP <150/80 (
NEJM
2008;358:1887) •
Lifestyle modifications
(each ↓ SBP ~5 mmHg)
weight loss: goal BMI 18.5–24.9; aerobic exercise: ≥30 min exercise/d, ≥5 d/wk
Other books
Stardust by Kanon, Joseph
The John Green Collection by Green, John
Good Morning Heartache by Audrey Dacey
Beyond the Orange Moon (Mathews Family Book 2) by Adrienne Frances
The Beast by Alianne Donnelly
Close Encounters by Kitt, Sandra
Mia's Dreams by Angelica Twilight
Flying Shoes by Lisa Howorth
The Paper Grail by James P. Blaylock
Backpacks and Bra Straps by Savannah Grace