Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (35 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
6.39Mb size Format: txt, pdf, ePub
• Daily awakening trial (d/c all sedation;
Lancet
2008;371:126): open eyes & w/o: agitation, RR >35, S
a
O
2
<88%, resp distress or arrhythmias (if fail, restart sedation at 1
/
2 prior dose).
• SBT = CPAP or T piece × 30–120 min
failure if: deteriorating ABGs, ↑ RR, ↑ or ↓ HR, ↑ or ↓ BP, diaphoresis, anxiety
• Tolerate SBT → extubation. Fail SBT → ? cause → work to correct → retry SBT qd
Complications
• Oxygen toxicity (theoretical); proportional to duration + degree of ↑ oxygen (F
i
O
2
>0.6)
• Ventilator-associated pneumonia (~1%/day, mortality rate ~30%)
typical pathogens: MRSA,
Pseudomonas
,
Acinetobacter
and
Enterobacter
species
preventive strategies (
AJRCCM
2005;171:388): wash hands, HOB elevated, non-nasal intub., enteral nutrition rather than TPN, routine suction of subglottic secretions, avoid unnecessary abx & transfusions, routine oral antiseptic, stress-ulcer prophylaxis w/ ? sucralfate (↓ VAP, ↑ GIB) vs. H
2
RA/PPI, ? silver-coated tubes (
JAMA
2008;300:805)
• Laryngeal
edema: for Pts vent >36 h; ? predicted bycuff leak test. Methylprednisolone 20 mg IV q4h starting 12 h pre-extub. → ↓↓ edema and 50% ↓ in reintubation (
Lancet
2007;369:1003)
ulceration: consider
tracheostomy
for patients in whom expect >14 d of mech vent → ↓ duration mech vent, ↓ # ICU days (
BMJ
2005;330:1243); no benefit to performing at ~1 wk vs. waiting until ~2 wk (
JAMA
2010;303:1483)
• Malnutrition (for all critically ill Pts):
enteral nutrition
initiated early is safe but not necessary (
JAMA
2012;307:795), but bolus may ↑ risk of VAP & C diff. (
JPEN
2002;26:174); no clear benefit to ✓ing gastric residuals (
JAMA
2013;309:249);
parenteral nutrition
should be delayed until after day 8 to ↓ risk of infections, cholestasis, RRT, ventilator days (
NEJM
2011;365:506)
• Oversedation/delirium: BDZs and polypharmacy are risk factors
propofol: HoTN in ~25%;
propofol infusion syndrome
(PRIS) ? esp. w/ high (>5 mg/kg/h) & prolonged (>48 h) infusions & concom vasopressors → ↑ AG, cardiac dysfxn, rhabdomyolysis, ↑ triglycerides, & renal failure (
Crit Care
2009;13:R169)
dexmedetomidine: ↑ vent-free days, but brady & HoTN c/w BDZ (
JAMA
2012;307:1151)
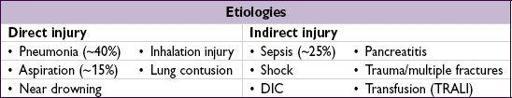
ACUTE RESPIRATORY DISTRESS SYNDROME
New “Berlin” definition
(
JAMA
2012;307:2526)
•
Acute onset
within 1 wk of clinical insult or worsening respiratory status
•
Bilateral infiltrates
without alternative explanation (eg, effusion, atelectasis, nodules)
•
Edema not fully explained
by fluid overload or congestive heart failure
•
Hypoxemia
: P
a
O
2
/F
i
O
2
determined with 5 cm H
2
O of PEEP
P
a
O
2
/F
i
O
2
200–300 = mild ARDS (may be on NIPPV), 100–200 = mod, <100 = severe
• Chest CT: heterogeneous lung with densities greater in dependent areas
• Lung bx: diffuse alveolar damage (DAD); Ø req, may give useful dx info (
Chest
2004;125:197)
Pathophysiology
• ↑ intrapulmonary shunt → hypoxemia (∴ Rx w/ PEEP to prevent derecruitment)
• ↑ increased dead space fraction (see Appendix), predicts ↑ mort. (
NEJM
2002;346:1281)
• ↓ compliance: V
T
/(P
plat
– PEEP) <50 mL/cm H
2
O
Treatment
(primarily supportive)
(
Lancet
2007;369:1553;
NEJM
2007;357:1113)
• Goal is to maintain gas exchange, sustain life, & avoid ventilator-induced lung injury (VILI)
•
Fluid balance
: target CVP 4–6 cm H
2
O (if nonoliguric & normotensive) → ↑ vent/ICU-free days, but no Δ mortality (
NEJM
2006;354:2564); PA catheter unproven (
NEJM
2006;354:2213); using BNP >200 to trigger diuresis (UOP goal 4.5–9 mL/kg/h × 3 h) ↓ time to extubation (
AJRCCM
2012;186:1256)
•
Steroids
: debate continues. Adverse effects include neuromuscular weakness, poor glc control, ? infection. Benefit may vary by time since ARDS onset:
<72 h: older studies w/o benefit (
NEJM
1987;317:1565); ? ↓ mortality, ↑ vent/ICU-free days in more recent, controversial study (
Chest
2007;131:954)
7–13 d: ? benefit → ↑ vent/ICU-free days, no mortality difference (
NEJM
2006;354:1671)
≥14 d: ↑ mortality (
NEJM
2006;354:1671)
•
Paralysis
: if P
a
O
2
/F
i
O
2
<150, cisatracurium × 48 h ↓ mortality (
NEJM
2010;363:1107)
•
Experimental
(
JAMA
2010;304:2521)
Inhaled NO or prostacyclins:
↑ P
a
O
2
/F
i
O
2
, no ↓ mort. or vent-free days (
BMJ
2007;334:779)
Prone
: ↑ P
a
O
2
, but ↑ complications and no ↓ mortality (
JAMA
2009;302:1977); ? ↓ mortality if P
a
O
2
/F
i
O
2
<100 (
Intens Care Med
2010;36:585)
High-freq oscillatory vent:
no benefit and possible harm (
NEJM
2013;368:795, 806, & 863)
Lung recruitment
: apply CPAP 40–45 cm H
2
O × 2 min to recruit lung and then ↑ PEEP to maintain; sicker Pts had ↑ recruitable lung (
NEJM
2006;354:1775, 1839)
ECMO:
may be useful in refractory ARDS, but no good trial data (
NEJM
2011;365:1905)
Esoph manometry:
adjust PEEP according to esoph pressure (pleural pressure) to maintain positive transpulm pressure → ↑ P
a
O
2
/F
i
O
2
, ↑ compliance and possible outcome benefit (
NEJM
2008;359:2095); helpful in obese Pts or w/ ↑ abdominal pressure
Prognosis
• Mortality ~40% overall in clinical trials; 9–15% resp. causes, 85–91% extrapulm (MODS)
• ↑ BNP & troponin a/w ↑ mortality (
Chest
2007;131:964;
PLoS One
2012;7:e40515)
• Survivors: PFTs ~normal, ↓ D
L
CO, muscle wasting, weakness persists (
NEJM
2003;348:683), ↓ exercise tolerance, ↓ QoL, ↑ psych morbidity (
NEJM
2011;364:1293)
SEPSIS
Other books
His Marriage Trap by Sheena Morrish
INTERVENTION by DENNIS MILLER
The All Encompassing: Shifter MC Novel (Pureblood Predator MC Book 1) by Daniels, May Ellis
01 Winters Thaw by Carr, Mari, Rylon, Jayne
Bill Rules by Elizabeth Fensham
Number Two by Jay Onrait
City of Bones by Cassandra Clare
Key Witness by Christy Barritt
State of Nature: Book Three of The Park Service Trilogy by Winfield, Ryan