Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (31 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
2.91Mb size Format: txt, pdf, ePub
spontaneous bacterial empyema (SBEM) can occur (even w/o SBP being present), ∴ thoracentesis if suspect infection
transplant is definitive treatment and workup should begin immediately
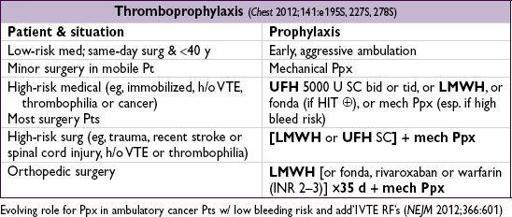
VENOUS THROMBOEMBOLISM (VTE)
Definitions
• Proximal deep venous thrombosis (DVT): thrombosis of popliteal, femoral or iliac veins
(nb, “superficial” femoral vein part of deep venous system)
• Pulmonary embolism (PE): thrombosis originating in venous system and embolizing to pulmonary arterial circulation; 1 case/1000 person y; 250,000/y (
Archives
2003;163:1711)
Risk factors
• Virchow’s triad for thrombogenesis
stasis
: bed rest, inactivity, CHF, CVA w/in 3 mo, air travel >6 h (
NEJM
2001;345:779)
injury to endothelium
: trauma, surgery, prior DVT, inflammation
thrombophilia
: APC resistance, protein C or S deficiency, APS, prothrombin gene mutation,↑ factor VIII, hyperhomocysteinemia, HIT, OCP, HRT, tamoxifen, raloxifene
• Malignancy (12% of “idiopathic” DVT/PE) • History of thrombosis (greater risk of recurrent VTE than genetic thrombophilia) • Statin therapy ↓ risk (
NEJM
2009;360:1851)
Clinical manifestations—DVT
• Calf pain, swelling (>3 cm c/w unaffected side), venous distention, erythema, warmth, tenderness, palpable cord,Homan’s sign (calf pain on dorsiflexion, seen in <5% of Pts),
phlegmasia cerulea dolens:
stagnant blood → edema,
cyanosis
, pain • 50% of Pts with sx DVT have asx PE
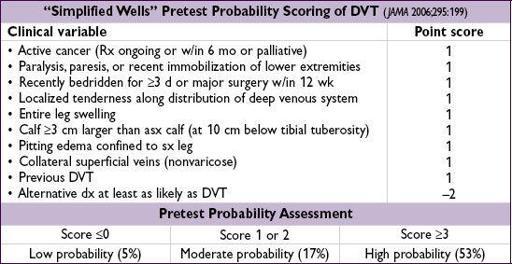
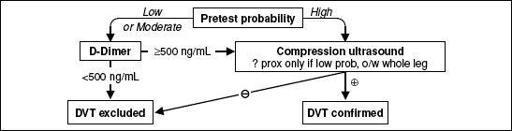
Diagnostic studies—DVT
• D-dimer: <500 helps r/o; ? use 1000 as threshold if low risk (
Annals
2013;158:93) • Compression U/S >95% Se & Sp for sx DVT (lower for asx DVT); survey whole leg rather than just proximal if ≥mod prob (
JAMA
2010;303:438); venography rarely used
Figure 2-3 Approach to suspected DVT (
Chest
2012;141:e351S)
Clinical manifestations—PE
• Dyspnea (73%), pleuritic chest pain (66%), cough (37%), hemoptysis (13%) • ↑ RR (>70%), crackles (51%), ↑ HR (30%), fever, cyanosis, pleural friction rub, loud P
2
•
Massive
: syncope, HoTN, PEA; ↑ JVP, R-sided S
3
, Graham Steell (PR) murmur
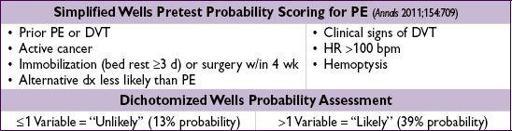
Diagnostic studies—PE
(
NEJM
2010;363:266)
• CXR (limited Se & Sp): 12% nl, atelectasis, effusion, ↑ hemidiaphragm, Hampton hump (wedge-shaped density abutting pleura); Westermark sign (avascularity distal to PE) • ECG (limited Se & Sp): sinus tachycardia, AF; signs of RV strain → RAD, P pulmonale, RBBB, S
I
Q
III
T
III
& TWI V
1
–V
4
(McGinn-White pattern,
Chest
1997;111:537) • ABG: hypoxemia, hypocapnia, respiratory alkalosis, ↑ A-a gradient (
Chest
1996;109:78) 18% w/ room air P
a
O
2
85–105 mmHg, 6% w/ nl A-a gradient (
Chest
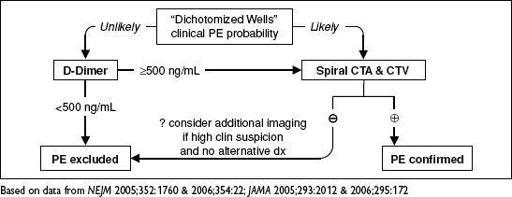
1991;100:598) • D-dimer: high Se, poor Sp (~25%);ELISA has >99% NPV and can be used to r/o PE in Pts w/ “unlikely” pretest prob. (
JAMA
2006;295:172) • Echocardiography: useful for risk stratification (RV dysfxn), but not dx (Se <50%) • V/Q scan: high Se (~98%), low Sp (~10%). Sp improves to 97% for high prob VQ. Use if pretest prob of PE high and CT not available or contraindicated. Can also exclude PE if low pretest prob, low prob VQ, but 4% false(
JAMA
1990;263:2753).
•
CT angiography
(CTA; see Radiology inserts): Se
90% & Sp
95% w/ MDCT (
NEJM
2006;354:2317); PPV & NPV >95% if imaging concordant w/ clinical suspicion, ≤80% if discordant (∴ need to consider both); CT may also provide other dx • Lower extremity compression U/S shows DVT in ~9%, sparing CTA, but when added to CTA, does not Δ outcomes (
Lancet
2008;371:1343) • Pulmonary angio: ? gold standard (morbidity 5%, mortality <0.5%), infrequently performed • MR angiography: Se 84% (segmental) to 100% (lobar) (
Lancet
2002;359:1643); if add MR venography, Se 92%, Sp 96% (
Annals
2010;152:434)
Figure 2-4 Approach to suspected PE using CTA
Workup for idiopathic VTE
•
Thrombophilia workup
: ✓ ifFH, consider if age <50 y or on OCP/HRT. Send panel 2 wk after complete anticoagulation, as thrombus, heparin and warfarin Δ results. Nb, does not change management after 1st idiopathic DVT if plan for long-term anticoagulation (
JAMA
2005;293:2352;
Blood
2008;112:4432;
Am J Med
2008;121:458).
Other books
I Don't Want To Kill You by Dan Wells
Cold as Ice by Charles Sheffield
The Edge of Chaos by Koke, Jak
Silvermay by James Moloney
Hot Pink by Adam Levin
Cracks in Reality (Seams in Reality Book 2) by Siegel, Alex
Wyvern and Company by Suttle, Connie
Glass Heart by Amy Garvey
Chasing Perfection Vol. 2 by Parker, M. S.
Zippered Flesh 2: More Tales of Body Enhancements Gone Bad by Bryan Hall, Michael Bailey, Shaun Jeffrey, Charles Colyott, Lisa Mannetti, Kealan Patrick Burke, Shaun Meeks, L.L. Soares, Christian A. Larsen