Resident Readiness General Surgery (17 page)
Read Resident Readiness General Surgery Online
Authors: Debra Klamen,Brian George,Alden Harken,Debra Darosa
Tags: #Medical, #Surgery, #General, #Test Preparation & Review

Answers
1.
A
. If we convert the VBG to an ABG, we can see that this patient has a metabolic acidosis. This reflects anaerobic metabolism, that is, end-organ hypoperfusion. Lethargy, while sensitive for cerebral hypoperfusion, is not specific—it could also be due to head trauma. Blood pressure and heart rate alone are not diagnostic unless they are associated with end-organ hypoperfusion.
2.
D
. You give volume until you are convinced the patient is at the peak of the Starling curve, based on blood pressure and/or cardiac output. Sometimes you will be able to normalize the blood pressure with volume alone, but you can imagine a scenario with a septic patient who cannot constrict his arterioles and might therefore remain hypotensive even if you’ve given him 50 L (and caused him to go into congestive heart failure).
3.
B
. It is counterintuitive, but this patient is not hypotensive for lack of arterial vasoconstriction. The patient is hypotensive because the heart cannot produce enough output. Increasing the afterload with pressors will reduce the already inadequate cardiac output by increasing the systemic vascular resistance that, in turn, decreases the stroke volume. The only time pressors might be indicated for a patient in shock is if there is peripheral vascular collapse from, say, sepsis or anaphylaxis.
SUGGESTED READING
Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock.
N Engl J Med
. 2001;345(19):1368–1377.
 A 67-year-old Man With Mental Status Changes and a Suspected Diverticular Abscess
A 67-year-old Man With Mental Status Changes and a Suspected Diverticular Abscess
Alexander T. Hawkins, MD, MPH
You are called to the emergency department to see a 67-year-old male for a suspected diverticular abscess. The EM resident tells you that “he’s starting to look sick” and you go immediately to see him. Vitals reveal a temperature of 102.7°F (39.3°C), pulse 102, blood pressure 90/50, a respiratory rate of 22, and an oxygen saturation of 96%. Physical exam reveals a somnolent male who grimaces when you palpate his abdomen. The nurse reports a clear mental status 1 hour prior. Stat labs reveal normal electrolytes and a leukocytosis of 17,000 WBC.
1.
Does this patient meet the diagnostic criteria for systemic inflammatory response syndrome (SIRS)?
2.
Does he meet the diagnostic criteria for sepsis?
3.
What features distinguish sepsis from severe sepsis?
4.
What features distinguish severe sepsis from septic shock?
5.
How would you obtain source control for this patient?
6. Name 3 other evidence-based interventions, besides source control, that you would do for this patient.
SEPSIS
Sepsis is a clinical syndrome characterized by a massive inflammatory response to infection. Over 650,000 cases of sepsis are diagnosed each year in the United States. Mortality is high and estimates range from 20% to 50% with rates increasing proportional to the severity of sepsis. Sepsis is thought to result from an overreaction of the immune response—a massive and uncontrolled release of proinflammatory mediators that leads to cardiovascular collapse and tissue injury. In its most severe form, sepsis can lead to multiorgan dysfunction syndrome (MODS) and subsequent death.
As sepsis is a clinical entity with a full spectrum of stages, much work has been done to codify and define its features.
Answers
1.
SIRS is the clinical syndrome that results from a dysregulated inflammatory response to an insult. It is nonspecific and can be caused by ischemia, inflammation, trauma, infection, or a combination of several insults.
This patient has SIRS. To establish the diagnosis of SIRS, 2 of the following criteria must be met:
•
High or low WBC (> 12,000 cells/mm
3
, <4000 cells/mm
3
, or >10% bands)
•
High or low temperature (>38.5°C or <35°C)
•
Heart rate >90
•
Respiratory rate >20 (or PaCO
2
<32 mm Hg)
2.
Sepsis is the clinical syndrome that results from the body’s abnormal inflammatory reaction to infection. Very simply:
Sepsis = SIRS + documented infection
This patient, in the absence of a documented infection, does not therefore have sepsis. Keep in mind that sepsis and bacteremia (bacteria in the bloodstream) are 2 different things. Patients can be bacteremic without being septic if they don’t meet diagnostic criteria for SIRS.
3.
Severe sepsis is defined by sepsis plus organ dysfunction (see
Figure 13-1
). This can be:
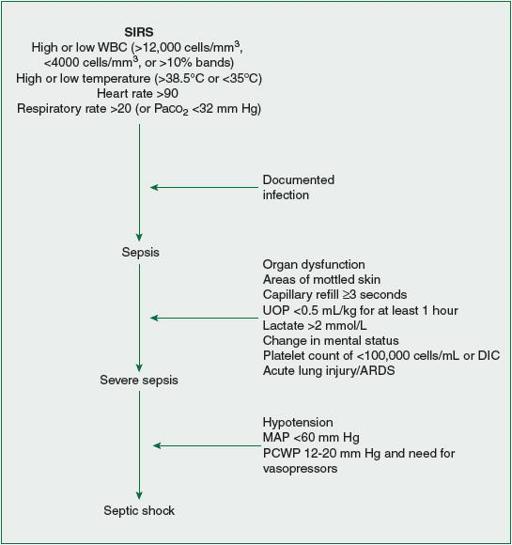
Figure 13-1.
The stepwise relationship between SIRS, sepsis, severe sepsis, and septic shock.
•
Areas of mottled skin
•
Capillary refill ≥3 seconds
•
UOP <0.5 mL/kg for at least 1 hour
•
Lactate >2 mmol/L
•
Change in mental status
•
Platelet count of <100,000 cells/mL or DIC
•
Acute lung injury/ARDS
4.
Septic shock is severe sepsis
plus
hypotension, which can include the following (see
Figure 13-1
):
•
MAP <60 mm Hg after fluid resuscitation
•
Pulmonary capillary wedge pressure between 12 and 20 mm Hg and need for vasopressors
5.
From the above definitions, for a patient to have sepsis there must be a source for the infection. This source can take the form of an abscess, infected tissue, perforated bowel, or any other place that bacteria can cause systemic effects. Source control relates to the need to eliminate the source of the original bacterial infection. This can mean percutaneous drainage of an abscess, wide debridement of infected tissue, or laparotomy and repair of a bowel perforation. In the case of our patient, source control means drainage of his abscess—through either open surgery or interventional radiology (IR) placement of a drain.
A.
Respiratory support
: The patient’s airway and ability to breathe should be assessed. Supplementary oxygen and pulse oximetry are mandatory for septic patients. Intubation and mechanical ventilation may be required both for the increased work of breathing that sepsis induces and to protect the airway of a somnolent and encephalopathic patient.
B.
Resuscitation and cardiovascular support
: Sepsis causes end-organ hypoperfusion through abnormal vasodilation (see the chapter on shock). Relative intravascular hypovolemia is common and needs to be addressed early in the course of the illness. This takes the form of central venous line placement followed by “goal-directed therapy.” “Goal-directed therapy” employs
guidelines to assist in proper resuscitation. Isotonic IV fluids (crystalloid) should be administered in boluses to achieve a central venous pressure (CVP) of between 8 and 12 mm Hg. If the patient remains hypotensive despite “filling up the tank,” then vasopressors need to be added to improve vascular tone. Norepinephrine and dopamine are the recommended vasopressors. If the patient remains in septic shock (as indicated by, eg, urine output less than 0.5 mL/kg/h, mixed venous saturation less than 65%, or continued metabolic acidosis), then inotropic support can be used to augment cardiac output. Although it is somewhat controversial, if the mixed venous saturation remains below 70%, then many will also transfuse a patient up to a hematocrit of 30%. Notice that this is essentially the same goal-directed therapy algorithm presented earlier, in the chapter on shock.
C.
Antibiotics
: While source control is critical, antibiotics also have an important role. Your antibiotic choice should be informed by local patterns of bacteria and drug resistance. Choose antibiotics that have a broad spectrum and good penetrance. Proper empirical therapies include carbapenems, third-or fourth-generation cephalosporins with additional anaerobic covers, or antipseudomonal penicillins. Vancomycin or linezolid should be employed if there is suspicion of methicillin-resistant
Staphylococcus aureus
.
D.
Other issues
: Adequate glycemic control (less than 180 mg/dL or 10 mmol/L) has been shown to improve mortality in sepsis and is an integral part of supportive care. See the chapter on perioperative insulin for more information on this topic.
Glucocorticoid use has been a major topic of research that has produced equivocal results as to the relative risks and benefits. For patients who are presently hypotensive despite maximum resuscitation, a trial of glucocorticoid steroids is appropriate.
Finally, nutritional support is an important part of the care of the septic patient. Unfortunately, consensus does not exist as to the method and timing of nutritional support.
In summary, a patient with sepsis should be transferred to and cared for in an intensive care unit. Time is of the essence and supportive treatment and antibiotics should be started as soon as you suspect a patient may have sepsis.
TIPS TO REMEMBER
SIRS = 2 of the following 4:
High or low WBC (>12k, <4k, or 10% bands)
