Ross & Wilson Anatomy and Physiology in Health and Illness (112 page)
Read Ross & Wilson Anatomy and Physiology in Health and Illness Online
Authors: Anne Waugh,Allison Grant
Tags: #Medical, #Nursing, #General, #Anatomy

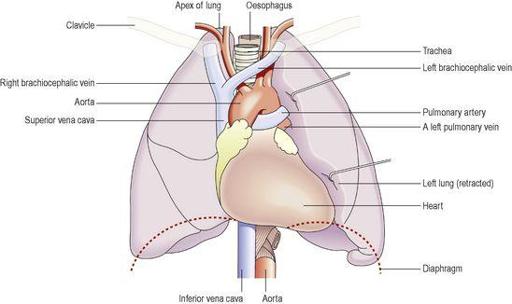
Position and gross structure (
Fig. 10.13
)
There are two lungs, one lying on each side of the midline in the thoracic cavity. They are cone-shaped and have an
apex
, a
base
, a
tip
,
costal surface
and
medial surface
.
Figure 10.13
Organs associated with the lungs.
The apex
This is rounded and rises into the root of the neck, about 25 mm above the level of the middle third of the clavicle. It lies close to the first rib and the blood vessels and nerves in the root of the neck.
The base
This is concave and semilunar in shape, and lies on the upper (thoracic) surface of the diaphragm.
The costal surface
This surface is convex and lies directly against the costal cartilages, the ribs and the intercostal muscles.
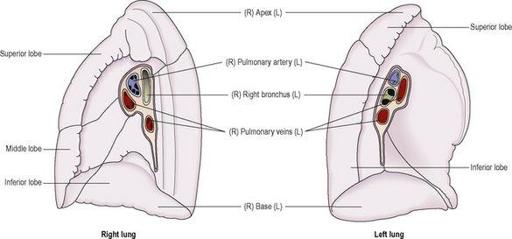
The medial surface
This surface is concave and has a roughly triangular-shaped area, called the
hilum
, at the level of the 5th, 6th and 7th thoracic vertebrae. Structures forming the
root of the lung
enter and leave at the hilum. These include the primary bronchus, the pulmonary artery supplying the lung and the two pulmonary veins draining it, the bronchial artery and veins, and the lymphatic and nerve supply (
Fig. 10.14
).
Figure 10.14
The lobes of the lungs and vessels/airways of each hilum
– medial views.
The area between the lungs is the
mediastinum
. It is occupied by the heart, great vessels, trachea, right and left bronchi, oesophagus, lymph nodes, lymph vessels and nerves.
The right lung is divided into three distinct lobes: superior, middle and inferior. The left lung is smaller because the heart occupies space left of the midline. It is divided into only two lobes: superior and inferior. The divisions between the lobes are called
fissures.
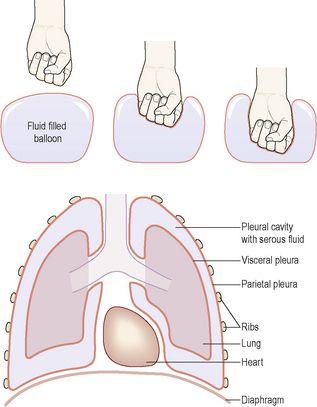
Pleura and pleural cavity
The pleura consists of a closed sac of serous membrane (one for each lung) which contains a small amount of serous fluid. The lung is invaginated (pushed into) into this sac so that it forms two layers: one adheres to the lung and the other to the wall of the thoracic cavity (
Figs 10.1
and
10.15
).
Figure 10.15
The relationship of the pleura to the lungs.
The visceral pleura
This is adherent to the lung, covering each lobe and passing into the fissures that separate them.
The parietal pleura
This is adherent to the inside of the chest wall and the thoracic surface of the diaphragm. It is not attached to other structures in the mediastinum and is continuous with the visceral pleura round the edges of the hilum.
The pleural cavity
This is only a potential space and contains no air. In health, the two layers of pleura are separated by a thin film of serous fluid (pleural fluid), which allows them to glide over each other, preventing friction between them during breathing. The serous fluid is secreted by the epithelial cells of the membrane. The double membrane arrangement of the pleura is similar to the serous pericardium of the heart (
p. 79
).
The two layers of pleura, with serous fluid between them, behave in the same way as two pieces of glass separated by a thin film of water. They glide over each other easily but can be pulled apart only with difficulty, because of the surface tension between the membranes and the fluid. If either layer of pleura is punctured, the underlying lung collapses owing to its inherent property of elastic recoil.
Interior of the lungs
The lungs are composed of the bronchi and smaller air passages, alveoli, connective tissue, blood vessels, lymph vessels and nerves, all embedded in an elastic connective tissue matrix. Each lobe is made up of a large number of
lobules
.
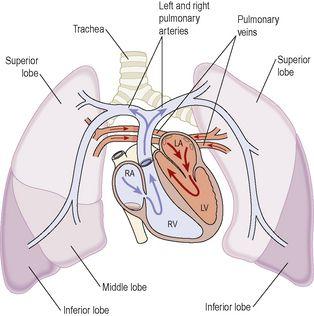
Pulmonary blood supply (
Fig. 10.16
)
The
pulmonary trunk
divides into the right and left pulmonary arteries, which transport deoxygenated blood to each lung. Within the lungs each pulmonary artery divides into many branches, which eventually end in a dense capillary network around the walls of the alveoli (see
Fig. 10.18
). The walls of the alveoli and the capillaries each consist of only one layer of flattened epithelial cells. The exchange of gases between air in the alveoli and blood in the capillaries takes place across these two very fine membranes (together called the
respiratory membrane
). The pulmonary capillaries join up, forming
two pulmonary veins
in each lung. They leave the lungs at the hilum and carry
oxygenated blood
to the left atrium of the heart. The innumerable blood capillaries and blood vessels in the lungs are supported by connective tissue.
Figure 10.16
The flow of blood between heart and lungs.
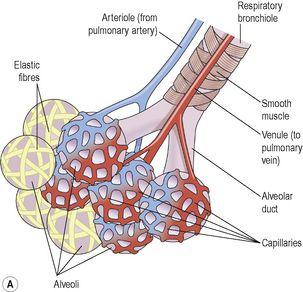
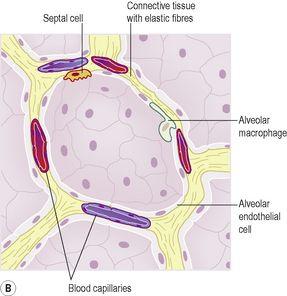
Figure 10.18
The alveoli and their capillary network. A.
A group of intact alveoli.
B.
Section through an alveolus.
The blood supply to the respiratory passages, lymphatic drainage and nerve supply is described later (
p. 245
).
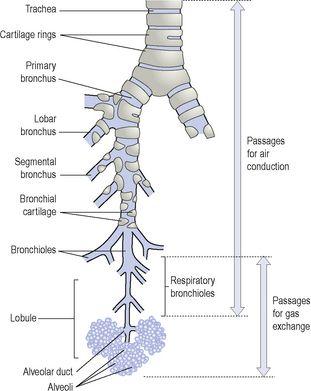
Bronchi and bronchioles
The two primary bronchi are formed when the trachea divides, at about the level of the 5th thoracic vertebra (
Fig. 10.17
).
Figure 10.17
The lower respiratory tract.
The right bronchus
This is wider, shorter and more vertical than the left bronchus and is therefore more likely to become obstructed by an inhaled foreign body. It is approximately 2.5 cm long. After entering the right lung at the hilum it divides into three branches, one to each lobe. Each branch then subdivides into numerous smaller branches.
The left bronchus
This is about 5 cm long and is narrower than the right. After entering the lung at the hilum it divides into two branches, one to each lobe. Each branch then subdivides into progressively smaller airways within the lung substance.
Structure