Ross & Wilson Anatomy and Physiology in Health and Illness (54 page)
Read Ross & Wilson Anatomy and Physiology in Health and Illness Online
Authors: Anne Waugh,Allison Grant
Tags: #Medical, #Nursing, #General, #Anatomy

relate the causes of oedema to relevant clinical problems
explain the causes and consequences of excess fluid collecting in body cavities.
In oedema, excess tissue fluid accumulates, causing swelling. It may occur either in superficial tissues or deeper organs.
Sites of oedema
When oedema is present in the superficial tissues,
pitting
of the surface may be observed, i.e. an indentation in the skin remains after firm finger pressure has been applied. The sites at which superficial oedema is observed are influenced by gravity and the position of the individual. When the individual is in the standing or sitting position the oedema is observed in the lower limbs, beginning in the feet and ankles. Patients on bedrest tend to develop oedema in the sacral area. This may be described as
dependent oedema
.
In
pulmonary oedema
, venous congestion in the lungs or increased pulmonary vessel permeability results in accumulation of fluid in the tissue spaces and in the alveoli. This reduces the area available for gaseous exchange and results in
dyspnoea
(breathlessness), cyanosis and coughing up (expectoration) of frothy sputum. The most common causes of pulmonary oedema are cardiac failure, inflammation or irritation of the lungs and excessive infusion of intravenous fluids.
Causes of oedema
Excess fluid accumulates in the tissues when some aspect of normal capillary fluid dynamics (
p. 77
) is deranged.
Increased venous hydrostatic (blood) pressure
Congestion of the venous circulation increases venous hydrostatic pressure, reducing the effect of osmotic pressure that draws fluid back into the capillary at the venous end. Excess fluid then remains in the tissues. This may be caused by heart failure, kidney disease or compression of a limb due to prolonged sitting or tight clothes.
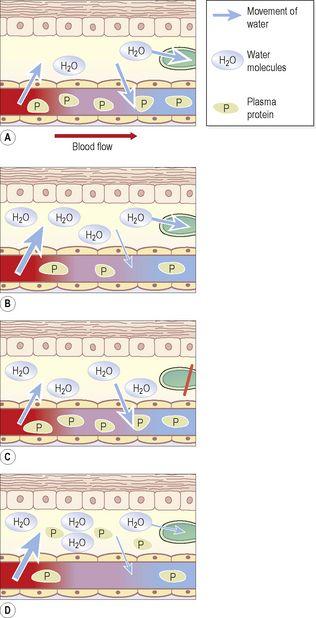
Decreased plasma osmotic pressure
When there is depletion of plasma proteins, less fluid returns to the circulation at the venous end of the capillary (
Fig. 5.61B
). Causes include excessive protein loss in kidney disease (
p. 344
), and reduced plasma protein levels caused by, for example, liver failure or a protein-deficient diet.
Figure 5.61
Capillary fluid dynamics. A.
Normal.
B.
Effect of reduced plasma proteins.
C.
Effect of impaired lymphatic drainage.
D.
Effect of increased capillary permeability. Arrows indicate direction of movement of water.
Impaired lymphatic drainage
Some fluid returns to the circulation via the lymphatic system and when flow is impaired, oedema develops (
Fig. 5.61C
). Causes include malignancy that blocks lymph drainage, surgical removal of lymph nodes or the destruction of lymph nodes by chronic inflammation.
Increased small-vessel permeability
In inflammation (
p. 367
), chemical mediators increase small vessel permeability in the affected area. Plasma proteins then leave the circulation (
Fig. 5.61D
) and the increased tissue osmotic pressure draws fluid into the area causing swelling of the affected tissue. This type of oedema also occurs in allergic reactions (
p. 374
), e.g. anaphylaxis, asthma or hay fever.
Ascites and effusions
Abnormal accumulation of excess fluid in body spaces, e.g. the pericardial sac or a joint space, is often associated with inflammatory, infective or obstructive conditions and is generally referred to as an
effusion
.
Ascites
This is the accumulation of excess fluid in the peritoneal cavity. The most common causes include liver failure (when plasma protein synthesis is reduced), obstruction of abdominal lymph nodes draining the peritoneal cavity, or inflammatory conditions. This includes malignant disease, because many tumours release pro-inflammatory mediators.
Pleural effusion
This is excess serous fluid in the pleural cavity. This is usually due to infection or inflammation of the pleura (
p. 243
), or to left ventricular failure, which increases pressure in the pulmonary circulation because the left ventricle is not able to pump out all the blood returning to it from the lungs.
Diseases of the heart
Learning outcomes
After studying this section, you should be able to:
describe the consequences of failure of either or both sides of the heart
explain the compensatory mechanisms that occur in heart failure
explain the causes and consequences of faulty heart valve function
define the term ischaemic heart disease
discuss the main conditions associated with ischaemic heart disease