Ross & Wilson Anatomy and Physiology in Health and Illness (52 page)
Read Ross & Wilson Anatomy and Physiology in Health and Illness Online
Authors: Anne Waugh,Allison Grant
Tags: #Medical, #Nursing, #General, #Anatomy

list the predisposing factors and the common sites of occurrence of varicose veins
describe the main tumours that affect blood vessels.
Atheroma
Pathological changes
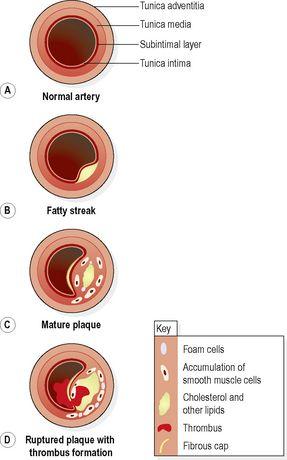
Atheromatous plaques
are patchy changes that develop in the tunica intima of large and medium-sized arteries. Initial changes show a fatty streak in the artery wall. Mature plaques consist of accumulations of cholesterol and other lipid compounds, excess smooth muscle and fat-filled monocytes (foam cells). The plaque is covered with a fibrous cap. As plaques grow they spread along the artery wall forming swellings that protrude into the lumen. Eventually the whole thickness of the wall and long sections of the vessel may be affected (
Fig. 5.57
). Plaques may rupture, exposing subintimal materials to the blood. This may cause thrombosis and vasospasm and will compromise blood flow.
Figure 5.57
Stages in the formation of an atheromatous plaque.
Arteries most commonly involved are those in the heart, brain, kidneys, small intestine and lower limbs.
Causes of atheroma
The origin of atheromatous plaques is uncertain.
Fatty streaks
present in artery walls of infants are usually absorbed but their incomplete absorption may be the origin of atheromatous plaques in later life.
Atherosclerosis
(the presence of plaques) is considered to be a disease of older people because it is usually in these age groups that clinical signs appear. Plaques, however, start to form in childhood in developed countries.
The incidence of atheroma is widespread in developed countries. Why atheromatous plaques develop is not clearly understood, but the predisposing factors appear to exert their effects over a long period. This may mean that the development of atheroma can be delayed or even arrested by a change in lifestyle (
Box 5.3
).
Box 5.3
Predisposing factors in atherosclerosis
(Modifiable factors are shown in green.)
•
Heredity – family history
•
Obesity
•
Gender – males are more susceptible than females, until after the female menopause
•
Diet – high in refined carbohydrates and/or saturated fats and cholesterol
•
Increasing age
•
Smoking cigarettes
•
Diabetes mellitus
•
Excessive emotional stress
•
Hypertension
•
Sedentary lifestyle
•
Hyperlipidaemia
•
Excessive alcohol consumption
Effects of atheroma
Atheromatous plaques may cause partial or complete obstruction of an artery. The blockage may be complicated by clot formation. The consequences of this depend on the site and size of the artery involved and the extent of collateral circulation. Commonly the arteries affected are those in the heart, abdomen and pelvis.
Narrowing of an artery
The tissues distal to the narrow point become ischaemic. The cells may receive enough blood to meet their minimum needs, but not enough to cope with an increase in metabolic rate, e.g. when muscle activity is increased. This causes acute cramp-like ischaemic pain, which disappears when exertion stops. Cardiac muscle and skeletal muscles of the lower limb are most commonly affected. Ischaemic pain in the heart is called
angina pectoris
(
p. 120
), and in the lower limbs,
intermittent claudication
.
Occlusion of an artery
When an artery is completely blocked, the tissues it supplies rapidly undergo degeneration and die from
ischaemia
, which leads to infarction. If a major artery supplying a large amount of tissue is affected, the consequences are likely to be more severe than if the obstruction occurs in a minor vessel. If the tissue is well provided with a collateral circulation (such as the circulus arteriosus provides in the brain), tissue damage is less than if there are few collateral vessels (which may be the case in the heart).
When a coronary artery is occluded
myocardial infarction
(
p. 121
) occurs. Occlusion of arteries in the brain causes cerebral ischaemia and this leads to
cerebral infarction
(stroke).
Complications of atheroma
Thrombosis and infarction (
p. 112
)
If the fibrous cap overlying a plaque breaks down, platelets are activated by the damaged cells and a blood clot forms, blocking the artery and causing ischaemia and infarction. Emboli may break off, travel in the bloodstream and lodge in small arteries distal to the clot, causing small infarcts.
Haemorrhage
Plaques may become calcified, making the artery brittle, rigid and unresponsive to rises in blood pressure. They may rupture, causing haemorrhage.
Aneurysm
When the arterial wall is weakened by spread of the plaque between the layers of tissue, a local dilation (aneurysm) may develop (see below). This may lead to thrombosis and embolism, or the aneurysm may rupture causing severe haemorrhage. The most common sites affected by atheroma are the aorta and the abdominal and pelvic arteries.
Arteriosclerosis
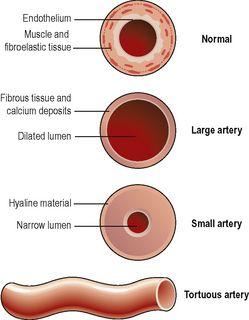
This is a progressive degeneration of arterial walls, associated with ageing and accompanied by hypertension.
In large and medium-sized arteries, the tunica media is infiltrated with fibrous tissue and calcium. This causes the vessels to become dilated, inelastic and tortuous (
Fig. 5.58
). Loss of elasticity increases systolic blood pressure, and the
pulse pressure
(the difference between systolic and diastolic pressure).