Ross & Wilson Anatomy and Physiology in Health and Illness (56 page)
Read Ross & Wilson Anatomy and Physiology in Health and Illness Online
Authors: Anne Waugh,Allison Grant
Tags: #Medical, #Nursing, #General, #Anatomy

A narrowed coronary artery may supply sufficient blood to the myocardium to meet its needs during rest or moderate exercise but not when greatly increased cardiac output is needed, e.g. walking may be tolerated but not running. The thick, inflexible atheromatous artery wall is unable to dilate to allow for the increased blood flow needed by the more active myocardium, which then becomes ischaemic. In the early stages of angina, the chest pain stops when the cardiac output returns to its resting level soon after the extra effort stops.
Myocardial infarction
The myocardium may infarct (
p. 113
) when a branch of a coronary artery is blocked. The commonest cause is an atheromatous plaque complicated by thrombosis. The extent of myocardial damage depends on the size of the blood vessel and site of the infarct. The damage is permanent because cardiac muscle cannot regenerate, and the dead muscle is replaced with non-functional fibrous tissue. Speedy restoration of blood flow through the blocked artery using clot-dissolving (thrombolytic) drugs can greatly reduce the extent of the permanent damage and improve prognosis, but treatment must be started within a few hours of the infarction occurring. The effects and complications are greatest when the left ventricle is involved.
Myocardial infarction is usually accompanied by very severe crushing chest pain behind the sternum which, unlike angina pectoris, continues even when the individual is at rest. It is a significant cause of death in the developed world.
Complications
These may be fatal and include:
•
severe arrhythmias, especially
ventricular fibrillation
(
p. 122
), due to disruption of the cardiac conducting system
•
acute heart failure (
p. 119
), caused by impaired contraction of the damaged myocardium and, in severe cases, cardiogenic shock
•
rupture of a ventricle wall, usually within 2 weeks of the original episode
•
pulmonary or cerebral embolism originating from a mural clot within a ventricle, i.e. a clot that forms inside the heart over the infarct
•
pericarditis
•
angina pectoris (
p. 120
)
•
recurrence.
Rheumatic heart disease
Rheumatic fever is an inflammatory illness that sometimes follows streptococcal throat infections, most commonly in children and young adults. It is an autoimmune disorder; the antibodies produced to combat the original infection damage connective tissues, including the heart, joints (
p. 424
) and skin.
Death rarely occurs in the acute phase, but after recovery there may be permanent damage to the heart valves, eventually leading to disability and possibly cardiac failure.
Acute rheumatic heart disease
In the acute stages, all layers of the heart wall are inflamed (
pancarditis
, ‘pan-’ meaning ‘all of’). The heart valves, especially the mitral valve, are frequently affected. Fibrotic nodules develop on their cusps, which shrink as they age, distorting the cusp and causing stenosis and incompetence of the valve. The inflamed myocardium can fail, leading to signs of heart failure, including tachycardia, breathlessness and cardiac enlargement. Inflammation of the pericardium can lead to friction within the pericardial cavity as the heart beats, pain behind the sternum and interference with the pumping action of the heart. Permanent fibrotic damage may fuse the visceral and parietal layers of the serous pericardium together, restricting the heart’s action.
Chronic rheumatic heart disease
Inflamed tissue becomes fibrous as it heals, and this fibrous tissue interferes with the action of the myocardium and the heart valves. At least half of acute cases develop chronic valvular incompetence following recovery. The great majority of these patients have mitral valve damage, but the aortic valve is frequently affected too. Chronic fibrotic changes in the pericardium and myocardium cause heart failure.
Sometimes rheumatic valvular disease presents with no history of acute rheumatic fever or streptococcal infection.
Infective endocarditis
Pathogenic organisms (usually bacteria or fungi) in the blood may colonise any part of the endocardium, but the most common sites are on or near the heart valves and round the margins of congenital heart defects. These areas are susceptible to infection because they are exposed to fast-flowing blood that may cause mild trauma. This is a serious illness and often fatal unless adequately treated.
The main predisposing factors are bacteraemia, depressed immune response and heart abnormalities.
Bacteraemia
Microbes in the bloodstream, if not destroyed by phagocytes or antibodies, tend to adhere to platelets and form tiny infected emboli. Inside the heart, the emboli are most likely to settle on already damaged endocardium. Vegetations consisting of platelets and fibrin surround the microbes and seem to protect them from normal body defences and antibiotics. Because of this, infection may be caused by a wide range of bacteria, including some that do not normally cause clinical infection. They normally originate from the skin or the mouth.
Depressed immune response
This enables low-virulence bacteria, viruses, yeasts and fungi to become established and cause infection. These are organisms always present in the body and the environment. Depression of the immune systems may be caused by HIV infection, malignant disease, cytotoxic drugs, radiotherapy or steroid therapy.
Heart abnormalities
The sites most commonly infected are already abnormal in some way. Pathogenic organisms present in the bloodstream cannot adhere to healthy endothelium, but if the endothelial lining of the cardiovascular system is damaged, infection is more likely. Often, the cardiac valves are involved, especially if damaged by rheumatic disease or congenital malformation. Other likely sites of infection include regions of cardiac abnormality, such as ventricular septal defect (
p. 124
) and patent ductus arteriosus (
p. 123
). Prosthetic (artificial) valves can also be a focus for infective growths.
Acute infective endocarditis
This is a severe febrile illness usually caused by high-virulence microbes, commonly
Staphylococcus aureus
. Vegetations grow rapidly and pieces may break off, becoming infected emboli. These settle in other organs where the microbes grow, destroying tissue and forming pus. The effects depend on the organ involved, e.g. brain or kidney infection may cause death in a few days. The causative microbes rapidly destroy heart valves, impairing their function and resulting in acute heart failure.
Subacute infective endocarditis
This endocarditis is usually caused by low-virulence microbes, e.g. non-haemolytic streptococci or some staphylococci. Infected emboli may settle in any organ but do not cause suppuration and rarely cause death. Microbes in the vegetations seem to be protected by surrounding platelets and fibrin from normal body defences and antibiotics. Healing by fibrosis further distorts the shape of the valve cusps, increasing the original stenosis and incompetence. Heart failure may develop later.
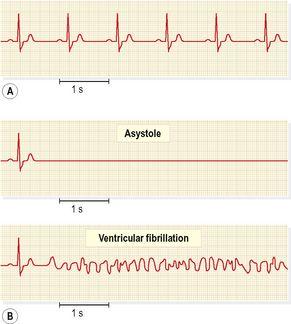
Cardiac arrhythmias
The heart rate is normally determined by intrinsic impulses generated in the SA node. The rhythm is determined by the route of impulse transmission through the conducting system. The heart rate is usually measured as the pulse, but to determine the rhythm, an electrocardiogram (ECG) is required (
Fig. 5.62A
). A
cardiac arrhythmia
is any disorder of heart rate or rhythm, and is the result of abnormal generation or conduction of impulses. The normal cardiac cycle (
p. 84
) gives rise to
normal sinus rhythm
, which has a rate of between 60 and 100 bpm.
Figure 5.62
ECG traces: A.
Normal sinus rhythm.
B.
Life-threatening arrhythmias.
Sinus bradycardia
This is normal sinus rhythm below 60 bpm. This may occur during sleep and is common in athletes. It is an abnormality when it follows myocardial infarction or accompanies raised intracranial pressure (
p. 172
).
Sinus tachycardia
This is normal sinus rhythm above 100 bpm when the individual is at rest. This accompanies exercise and anxiety, but is an indicator of some disorders, e.g. fever, hyperthyroidism, some cardiac conditions.
Asystole
This occurs when there is no electrical activity in the ventricles and therefore no cardiac output. The ECG shows a flat line (
Fig. 5.62B
). Ventricular fibrillation and asystole cause sudden and complete loss of cardiac output, i.e.
cardiac arrest
and death.
Fibrillation
This is the contraction of the cardiac muscle fibres in a disorderly sequence. The chambers do not contract as a coordinated unit and the pumping action is disrupted.
In
atrial fibrillation
, contraction of the atria is uncoordinated and rapid, pumping is ineffective and stimulation of the AV node is disorderly. Ventricular contraction becomes rapid and rhythm and force irregular; although an adequate cardiac output and blood pressure may be maintained, the pulse is irregular. The causes of increased excitability and disorganised activity are not always clear but predisposing conditions include:
•
ischaemic heart disease (
p. 120
)
•
degenerative changes in the heart due to old age
•
thyrotoxicosis (
p. 222
)
•
rheumatic heart disease (
p. 121
).
Ventricular fibrillation
is a medical emergency that will swiftly lead to death if untreated, because the chaotic electrical activity within the ventricular walls cannot coordinate effective pumping action (cardiac arrest).
Blood is not pumped from the heart into either the pulmonary or the systemic circulation. No pulses can be felt, consciousness is lost and breathing stops. The ECG shows an irregular chaotic trace with no recognisable wave pattern (
Fig. 5.62B
).
Heart block
Heart block occurs when normal impulse transmission is blocked or impaired. A common form involves obstruction of impulse transmission through the AV node, but (less commonly) conducting tissue in the atria or ventricles can also be affected. When the AV node is involved, the delay between atrial and ventricular contraction is increased. The severity depends on the extent of loss of stimulation of the AV node.
In
complete heart block
, ventricular contraction is entirely independent of impulses initiated by the SA node. Freed from the normal pacing action of the SA node, the ventricles are driven by impulses generated by the pacemaker activity of the AV node, resulting in slow, regular ventricular contractions and a heart rate of about 30 to 40 beats per minute. In this state the heart is unable to respond quickly to a sudden increase in demand by, for example, muscular exercise. The most common causes are:
•
acute ischaemic heart disease
•
myocardial fibrosis following repeated infarctions or myocarditis
•
drugs used to treat heart disease, e.g. digitalis, propranolol.
When heart block develops gradually there is some degree of adjustment in the body to reduced cardiac output but, if progressive, it eventually leads to death from cardiac failure and cerebral anoxia.
Congenital abnormalities
Abnormalities in the heart and great vessels at birth may be due to intrauterine developmental errors or to the failure of the heart and blood vessels to adapt to extrauterine life. Sometimes, there are no symptoms in early life and the abnormality is recognised only when complications appear.
Patent ductus arteriosus
Before birth the ductus arteriosus, joining the arch of the aorta and the pulmonary artery, allows blood to pass from the pulmonary artery to the aorta (
Figs 5.53
and
5.63
). It carries blood pumped into the pulmonary trunk by the right ventricle into the aorta, bypassing the pulmonary circulation, which in the unborn child is not functional because the fetus derives his oxygen supply through the placenta. At birth, when the pulmonary circulation is established, the ductus arteriosus should close completely. If it remains patent, blood regurgitates from the aorta to the pulmonary artery where the pressure is lower, reducing the volume entering the systemic circulation and increasing the volume of blood in the pulmonary circulation. This leads to pulmonary congestion and eventually cardiac failure.