Ross & Wilson Anatomy and Physiology in Health and Illness (155 page)
Read Ross & Wilson Anatomy and Physiology in Health and Illness Online
Authors: Anne Waugh,Allison Grant
Tags: #Medical, #Nursing, #General, #Anatomy

Chronic cholecystitis
The onset is usually insidious, sometimes following repeated acute attacks. Gallstones are invariably present and there may be accompanying biliary colic. Pain is due to the spasmodic contraction of muscle, causing ischaemia when the gall bladder is packed with gallstones. There is usually secondary infection with suppuration. Ulceration of the tissues between the gall bladder and the duodenum or colon may occur with fistula formation and, later, fibrous adhesions.
Cholangitis
This is inflammation of bile ducts in which there is partial or complete obstruction by gallstones. Complete obstruction of the common bile duct causes acute cholangitis, which is typically accompanied by biliary colic, fever and jaundice (because the flow of bile into the duodenum is blocked). In practice, not all of these symptoms are usually present. This situation predisposes to secondary infection which can spread upwards in the biliary tree to the liver (
ascending cholangitis
) causing liver abscesses.
Tumours of the biliary tract
Benign tumours are rare.
Malignant tumours
These are relatively rare and gallstones are nearly always present. Local spread to the liver, the pancreas and other adjacent organs is common. Lymph and blood spread lead to widespread metastases. The tumour has often spread by the time of diagnosis and, therefore, the prognosis is poor.
Jaundice
This is not a disease in itself, but yellowing of the skin and mucous membrane is a sign of abnormal bilirubin metabolism and excretion. Bilirubin, produced from the breakdown of haemoglobin, is normally conjugated in the liver and excreted in the bile (
Fig. 12.37
). Conjugation, the process of adding certain groups to the bilirubin molecule, makes it water-soluble and greatly enhances its removal from the blood, an essential step in excretion.
Unconjugated bilirubin, which is fat-soluble, has a toxic effect on brain cells. However, it is unable to cross the blood–brain barrier until the plasma level rises above 340 μmol/l, but when it does it may cause neurological damage, seizures (fits) and mental impairment. Serum bilirubin may rise to 40 to 50 μmol/l before the yellow coloration of jaundice is evident in the skin and conjunctiva (normal 3 to 13 μmol/l). Jaundice is often accompanied by
pruritus
(itching) caused by the irritating effects of bile salts on the skin.
Jaundice develops when there is an abnormality of bilirubin processing and the different types are considered below.
Types of jaundice
Whatever stage in bilirubin processing is affected, the end result is rising blood bilirubin levels.
Pre-hepatic jaundice
This is due to increased haemolysis of red blood cells (see
Fig. 12.37 and p. 59
) that results in production of excess bilirubin. Because the excess bilirubin is unconjugated it cannot be excreted in the urine, which therefore remains normal in colour.
Neonatal haemolytic jaundice
occurs in many babies, especially in those born prematurely where the normal high haemolysis is coupled with shortage of conjugating enzymes in the hepatocytes of the still immature liver.
Intra-hepatic jaundice
This is the result of damage to the liver itself by, e.g.:
•
viral hepatitis (
p. 324
)
•
toxic substances, such as drugs
•
amoebiasis (amoebic dysentery) (
p. 319
)
•
cirrhosis (
p. 325
).
Excess bilirubin accumulates in the liver. Because it is mainly in the conjugated form, it is water-soluble and excreted in the urine making it dark in colour.
Post-hepatic jaundice
Causes of obstruction to the flow of bile in the biliary tract include:
•
gallstones in the common bile duct
•
tumour of the head of the pancreas
•
fibrosis of the bile ducts, following cholangitis or injury by the passage of gallstones.
In this situation excess bilirubin is also conjugated and is therefore excreted in the urine. The effects of raised serum bilirubin include:
•
pruritus (itching)
•
pale faeces due to absence of stercobilin (
p. 296
)
•
dark urine due to the presence of increased amounts of bilirubin.
For a range of self-assessment exercises on the topcs in this chapter, visit
www.rossandwilson.com
.
CHAPTER 13
The urinary system
Kidneys
330
Organs associated with the kidneys
331
Gross structure of the kidney
331
Microscopic structure of the kidney
331
Functions of the kidney
334
Ureters
338
Structure
339
Function
339
Urinary bladder
339
Organs associated with the bladder
339
Structure
339
Urethra
340
Micturition
341
Diseases of the kidneys
343
Glomerulonephritis (GN)
343
Nephrotic syndrome
344
Diabetic nephropathy
345
Hypertension and the kidneys
345
Acute pyelonephritis
345
Reflux nephropathy
345
Renal failure
345
Renal calculi
347
Congenital abnormalities of the kidneys
347
Tumours of the kidney
348
Diseases of the renal pelvis, ureters, bladder and urethra
348
Obstruction to the outflow of urine
348
Urinary tract infections (UTIs)
349
Tumours of the bladder
349
Urinary incontinence
349
ANIMATIONS
13.1
The urinary system
330
13.2
Gross structure of the kidney
331
13.3
Structure of the nephron
331
13.4
Filtration
334
13.5
Renal filtration
334
13.6
Reabsorption
335
13.7
Aldosterone regulation mechanism
335
13.8
Secretion
336
13.9
Urinary mechanism of pH control
338
13.10
Ureters
339
13.11
Bladder
339
13.12
Urethra
341
13.13
Renal stone
347
13.14
Hydroureter
347
13.15
Hydronephrosis
348
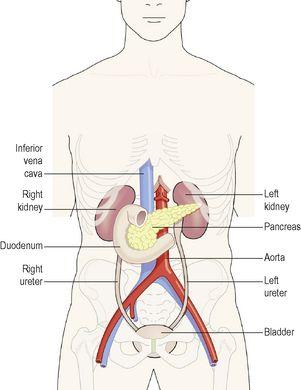
The urinary system is the main excretory system and consists of the following structures:
•
2
kidneys
, which secrete urine
•
2
ureters
, which convey the urine from the kidneys to the urinary bladder
•
the
urinary bladder
where urine collects and is temporarily stored
•
the
urethra
through which the urine passes from the urinary bladder to the exterior.
Figure 13.1
shows an overview of the urinary system.