Ross & Wilson Anatomy and Physiology in Health and Illness (158 page)
Read Ross & Wilson Anatomy and Physiology in Health and Illness Online
Authors: Anne Waugh,Allison Grant
Tags: #Medical, #Nursing, #General, #Anatomy

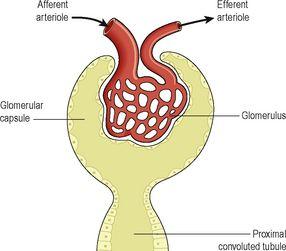
Figure 13.11
Filtration in the glomerulus.
Figure 13.10
The glomerulus and glomerular capsule.
Box 13.1
Constituents of glomerular filtrate and glomerular capillaries
| Blood constituents in glomerular filtrate | Blood constituents remaining in glomerular capillaries |
| Water | Leukocytes |
| Mineral salts | Erythrocytes |
| Amino acids | Platelets |
| Ketoacids | Plasma proteins |
| Glucose | Some drugs (large molecules) |
| Some hormones | |
| Creatinine | |
| Urea | |
| Uric acid | |
| Some drugs (small molecules) |
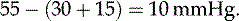
Filtration takes place because there is a difference between the blood pressure in the glomerulus and the pressure of the filtrate in the glomerular capsule. Because the efferent arteriole is narrower than the afferent arteriole, a
capillary hydrostatic pressure
of about 7.3 kPa (55 mmHg) builds up in the glomerulus. This pressure is opposed by the
osmotic pressure
of the blood, provided mainly by plasma proteins, about 4 kPa (30 mmHg), and by
filtrate hydrostatic pressure
of about 2 kPa (15 mmHg) in the glomerular capsule. The net
filtration pressure
is, therefore:

The volume of filtrate formed by both kidneys each minute is called the
glomerular filtration rate
(GFR). In a healthy adult the GFR is about 125 ml/min, i.e. 180 litres of filtrate are formed each day by the two kidneys. Nearly all of the filtrate is later reabsorbed from the kidney tubules with less than 1%, i.e. 1 to 1.5 litres, excreted as urine. The differences in volume and concentration are due to selective reabsorption of some filtrate constituents and tubular secretion of others.
Autoregulation of filtration
Renal blood flow is protected by a mechanism called
autoregulation
, whereby renal blood flow is maintained at a constant pressure across a wide range of systolic blood pressures (from around 80 to 200 mmHg). Autoregulation operates independently of nervous control, i.e. if the nerve supply to the renal blood vessels is interrupted, autoregulation continues to operate. It is therefore a property inherent in renal blood vessels; it may be stimulated by changes in blood pressure in the renal arteries or by fluctuating levels of certain metabolites, e.g. prostaglandins.
In severe shock, when the systolic blood pressure falls below 80 mmHg, autoregulation fails and renal blood flow and the hydrostatic pressure decrease, impairing filtration within the nephrons.
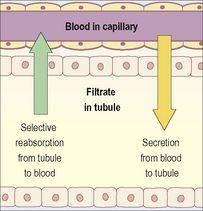
Selective reabsorption (
Fig. 13.12
)
Most reabsorption from the filtrate back into the blood takes place in the proximal convoluted tubule, whose walls are lined with microvilli to increase surface area for absorption. Materials essential to the body are reabsorbed here, including some water, electrolytes and organic nutrients such as glucose. Some reabsorption is passive, but some substances are transported actively. Only 60–70% of filtrate reaches the loop of the nephron. Much of this, especially water, sodium and chloride, is reabsorbed in the loop, so only 15–20% of the original filtrate reaches the distal convoluted tubule, and the composition of the filtrate is now very different from its starting values. More electrolytes are reabsorbed here, especially sodium, so the filtrate entering the collecting ducts is actually quite dilute. The main function of the collecting ducts therefore is to reabsorb as much water as the body needs.
Figure 13.12
Directions of selective reabsorption and secretion in the nephron.
Active transport takes place at carrier sites in the epithelial membrane, using chemical energy to transport substances against their concentration gradients (
p. 32
).
Some ions, e.g. sodium and chloride, can be absorbed by both active and passive mechanisms depending on the site in the nephron.
Some constituents of glomerular filtrate (e.g. glucose, amino acids) do not normally appear in urine because they are completely reabsorbed unless blood levels are excessive.
Reabsorption of nitrogenous waste products, such as urea, uric acid and creatinine is very limited.
The kidneys’ maximum capacity for reabsorption of a substance is the
transport maximum
, or renal threshold. For example, the normal blood glucose level is 3.5 to 8 mmol/l (63 to 144 mg/100 ml) and if this rises above the transport maximum of about 9 mmol/l (160 mg/100 ml), glucose appears in the urine. This occurs because all the carrier sites are occupied and the mechanism for active transport out of the tubules is overloaded. Other substances reabsorbed by active transport include sodium, calcium, potassium, phosphate and chloride.
The transport maximum, or renal threshold, of some substances varies according to body need at a particular time, and in some cases reabsorption is regulated by hormones.
Hormones that influence selective reabsorption
Parathyroid hormone
This comes from the parathyroid glands and together with
calcitonin
from the thyroid gland regulates the reabsorption of calcium and phosphate from the distal collecting tubules.
Antidiuretic hormone
Also known as ADH, this is secreted by the posterior lobe of the pituitary gland and increases the permeability of the distal convoluted tubules and collecting tubules, increasing water reabsorption. Secretion of ADH is controlled by a negative feedback system (
Fig. 13.13
).