Ross & Wilson Anatomy and Physiology in Health and Illness (206 page)
Read Ross & Wilson Anatomy and Physiology in Health and Illness Online
Authors: Anne Waugh,Allison Grant
Tags: #Medical, #Nursing, #General, #Anatomy

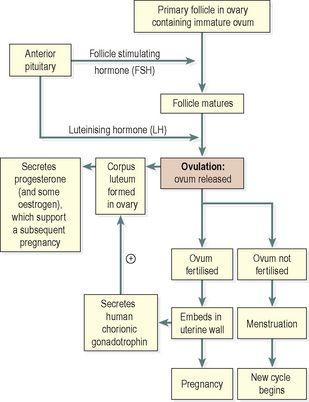
The hypothalamus secretes luteinising hormone releasing hormone (LHRH), which stimulates the anterior pituitary to secrete (see
Table 9.1, p. 211)
:
•
follicle stimulating hormone (FSH), which promotes the maturation of ovarian follicles and the secretion of oestrogen, leading to ovulation. FSH is therefore predominantly active in the first half of the cycle. Its secretion is suppressed once ovulation has taken place, to prevent other follicles maturing during the current cycle
•
luteinising hormone (LH), which triggers ovulation, stimulates the development of the corpus luteum and the secretion of progesterone.
The hypothalamus responds to changes in the blood levels of oestrogen and progesterone. It is stimulated by high levels of oestrogen alone (as happens in the first half of the cycle) but suppressed by oestrogen and progesterone together (as happens in the second half of the cycle).
The average length of the cycle is about 28 days. By convention the days of the cycle are numbered from the beginning of the
menstrual phase
, which usually lasts about 4 days. This is followed by the
proliferative phase
(about 10 days), then by the
secretory phase
(about 14 days).
Menstrual phase
When the ovum is not fertilised, the corpus luteum starts to degenerate. (In the event of pregnancy, the corpus luteum is supported by human chorionic gonadotrophin (hCG) secreted by the developing embryo). Progesterone and oestrogen levels therefore fall, and the functional layer of the endometrium, which is dependent on high levels of these ovarian hormones, is shed in menstruation (
Fig. 18.10C
). The menstrual flow consists of the secretions from endometrial glands, endometrial cells, blood from the degenerating capillaries and the unfertilised ovum.
High circulating levels of ovarian progesterone and oestrogen inhibit the anterior pituitary, blocking the release of FSH and LH, and should pregnancy occur then rising oestrogen and progesterone levels therefore prevent the maturation and release of another ovum. After degeneration of the corpus luteum, however, falling levels of oestrogen and progesterone lead to resumed anterior pituitary activity, rising FSH levels and the initiation of the next cycle.
Proliferative phase
At this stage an ovarian follicle, stimulated by FSH, is growing towards maturity and is producing oestrogen, which stimulates proliferation of the functional layer of the endometrium in preparation for the reception of a fertilised ovum. The endometrium thickens, becoming very vascular and rich in mucus-secreting glands. Rising levels of oestrogen are responsible for triggering a surge of LH approximately mid-cycle. This LH surge triggers ovulation, marking the end of the proliferative phase.
Secretory phase
After ovulation, LH from the anterior pituitary stimulates development of the corpus luteum from the ruptured follicle, which produces progesterone and some oestrogen. Under the influence of progesterone, the endometrium becomes oedematous and the secretory glands produce increased amounts of watery mucus. This is believed to assist the passage of the spermatozoa through the uterus to the uterine tubes where the ovum is usually fertilised. There is a similar increase in the secretion of watery mucus by the glands of the uterine tubes and by cervical glands that lubricate the vagina.
The ovum may survive in a fertilisable form for a very short time after ovulation, probably as little as 8 hours. The spermatozoa, deposited in the vagina during intercourse, may be capable of fertilising the ovum for only about 24 hours although they can survive for several days. This means that the period in each cycle during which fertilisation can occur is relatively short. Observable changes in the woman’s body occur around the time of ovulation. Cervical mucus, normally thick and dry, becomes thin, elastic and watery, and body temperature rises by a small but measurable amount immediately following ovulation. Some women experience abdominal discomfort in the middle of the cycle, thought to correspond to rupture of the follicle and release of its contents into the abdominal cavity.
If the ovum is not fertilised, the corpus luteum degenerates and dies, menstruation occurs and a new cycle begins.
If the ovum is fertilised there is no breakdown of the endometrium and no menstruation. The fertilised ovum (zygote) travels through the uterine tube to the uterus where it becomes embedded in the wall and produces human chorionic gonadotrophin (hCG), which is similar to anterior pituitary luteinising hormone. This hormone keeps the corpus luteum intact, enabling it to continue secreting progesterone and oestrogen for the first 3 to 4 months of the pregnancy, inhibiting the maturation of further ovarian follicles (
Figure 18.11
). During that time the placenta develops and produces oestrogen, progesterone and gonadotrophins.

Figure 18.11
Summary of the stages of development of the ovum and the associated hormones.
This is summarised in
Figure 18.11
.
Box 18.1
summarises the reproductive functions of oestrogen and progesterone.
Box 18.1
Reproductive functions of oestrogen and progesterone
Oestrogen
•
Development of secondary sexual characteristics at puberty
•
Stimulates and supports thickening of uterine lining during proliferative phase
•
Triggers LH surge mid-cycle, stimulating ovulation
•
Stimulates anterior pituitary secretion of FSH and LH in first half of cycle
Progesterone
•
Stimulates and supports thickening and increased glandular development of uterine lining during secretory phase
•
With oestrogen, inhibits secretion of FSH and LH from the anterior pituitary in second half of cycle
Menopause
The menopause (climacteric) usually occurs between the ages of 45 and 55 years, marking the end of the childbearing period. It may occur suddenly or over a period of years, sometimes as long as 10 years, and is caused by a progressive reduction in oestrogen levels, as the number of functional follicles in the ovaries declines with age. The ovaries gradually become less responsive to FSH and LH, and ovulation and the menstrual cycle become irregular, eventually ceasing. Several other phenomena may occur at the same time, including:
•
short-term unpredictable vasodilation with flushing, sweating and palpitations, causing discomfort and disturbance of the normal sleep pattern
•
shrinkage of the breasts
•
axillary and pubic hair become sparse
•
atrophy of the sex organs
•
episodes of uncharacteristic behaviour, e.g. irritability, mood changes
•
gradual thinning of the skin
•
loss of bone mass predisposing to osteoporosis (
p. 421
)
•
slow increase in blood cholesterol levels that increase the risk of cardiovascular disease in postmenopausal women to that in males of the same age.
Similar changes occur after bilateral irradiation or surgical removal of the ovaries.
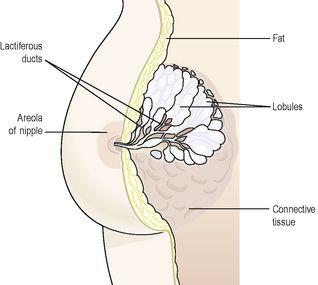
Breasts
The breasts or
mammary glands
are accessory glands of the female reproductive system. They exist also in the male, but in only a rudimentary form.
Structure
The mammary glands or breasts (
Fig 18.12
) consist of varying amounts of glandular tissue, responsible for milk production, supported by fatty tissue and fibrous connective tissue that anchor the breast to the chest wall.