Ross & Wilson Anatomy and Physiology in Health and Illness (208 page)
Read Ross & Wilson Anatomy and Physiology in Health and Illness Online
Authors: Anne Waugh,Allison Grant
Tags: #Medical, #Nursing, #General, #Anatomy

Figure 18.14
The testis: A.
Section of the testis and its coverings.
B.
Longitudinal section of a testis and deferent duct.
Tunica vaginalis
This is a double membrane, forming the outer covering of the testes, and is a downgrowth of the abdominal and pelvic peritoneum. During early fetal life, the testes develop in the lumbar region of the abdominal cavity just below the kidneys. They then descend into the scrotum, taking with them coverings of peritoneum, blood and lymph vessels, nerves and the deferent duct. The peritoneum eventually surrounds the testes in the scrotum, and becomes detached from the abdominal peritoneum. Descent of the testes into the scrotum should be complete by the 8th month of fetal life.
Tunica albuginea
This is a fibrous covering beneath the tunica vaginalis that surrounds the testes. Ingrowths form septa, dividing the glandular structure of the testes into
lobules
.
Tunica vasculosa
This consists of a network of capillaries supported by delicate connective tissue.
Structure
In each testis are 200 to 300 lobules, and within each lobule are 1 to 4 convoluted loops composed of
germinal epithelial cells
, called
seminiferous tubules
. Between the tubules are groups of
interstitial cells
(
of Leydig
) that secrete the hormone testosterone after puberty. At the upper pole of the testis the tubules combine to form a single tubule. This tubule, about 6 m in its full length, is repeatedly folded and tightly packed into a mass called the epididymis. It leaves the scrotum as the
deferent duct
(vas deferens) in the spermatic cord. Blood and lymph vessels pass to the testes in the
spermatic cords
.
Functions
Spermatozoa (sperm) are produced in the seminiferous tubules of the testes, and mature as they pass through the long and convoluted epididymis, where they are stored. The hormone controlling sperm production is FSH from the anterior pituitary (
p. 211
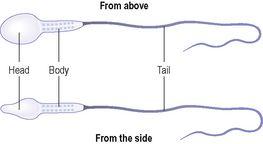
). A mature sperm (
Fig. 18.15
) has a head, a body, and a long whip-like tail used for motility. The head is almost completely filled by the nucleus, containing its DNA. It also contains the enzymes required to penetrate the outer layers of the ovum to reach, and fuse with, its nucleus. The body of the sperm is packed with mitochondria, to fuel the propelling action of the tail that powers the sperm along the female reproductive tract.
Figure 18.15
A spermatozoon.
Successful spermatogenesis takes place at a temperature about 3°C below normal body temperature. The testes are cooled by their position outside the abdominal cavity, and the thin outer covering of the scrotum has very little insulating fat.
Spermatic cords
The spermatic cords suspend the testes in the scrotum. Each cord contains a testicular artery, testicular veins, lymphatics, a deferent duct and testicular nerves, which come together to form the cord from their various origins in the abdomen. The cord, which is covered in a sheath of smooth muscle and connective and fibrous tissues, extends through the inguinal canal (
p. 416
) and is attached to the testis on the posterior wall.
Blood supply, lymph drainage and nerve supply
Arterial supply
The testicular artery branches from the abdominal aorta, just below the renal arteries.
Venous drainage
The testicular vein passes into the abdominal cavity. The left vein opens into the left renal vein and the right into the inferior vena cava.
Lymph drainage
This is through lymph nodes around the aorta.
Nerve supply
This is provided by branches from the 10th and 11th thoracic nerves.
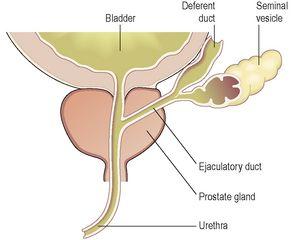
The deferent duct
This is some 45 cm long. It passes upwards from the testis through the inguinal canal and ascends medially towards the posterior wall of the bladder where it is joined by the duct from the seminal vesicle to form the
ejaculatory duct
(
Fig. 18.16
).
Figure 18.16
Section of the prostate gland and associated reproductive structures on one side.
Seminal vesicles
The seminal vesicles are two small fibromuscular pouches lined with columnar epithelium, lying on the posterior aspect of the bladder (
Fig. 18.16
).
At its lower end each seminal vesicle opens into a short duct, which joins with the corresponding deferent duct to form an ejaculatory duct.
Functions
The seminal vesicles contract and expel their stored contents, seminal fluid, during ejaculation. Seminal fluid, which forms 60% of the bulk of the fluid ejaculated at male orgasm, contains nutrients to support the sperm during their journey through the female reproductive tract.
Ejaculatory ducts
The ejaculatory ducts are two tubes about 2 cm long, each formed by the union of the duct from a seminal vesicle and a deferent duct. They pass through the prostate gland and join the prostatic urethra, carrying seminal fluid and spermatozoa to the urethra (
Fig. 18.16
).
The ejaculatory ducts are composed of the same layers of tissue as the seminal vesicles.
Prostate gland
The prostate gland (
Fig. 18.16
) lies in the pelvic cavity in front of the rectum and behind the symphysis pubis, surrounding the first part of the urethra. It consists of an outer fibrous covering, a layer of smooth muscle and glandular substance composed of columnar epithelial cells.
Functions
The prostate gland secretes a thin, milky fluid that makes up about 30% of
semen
, and gives it its milky appearance. It contains a clotting enzyme, which thickens the semen in the vagina, increasing the likelihood of semen being retained close to the cervix.
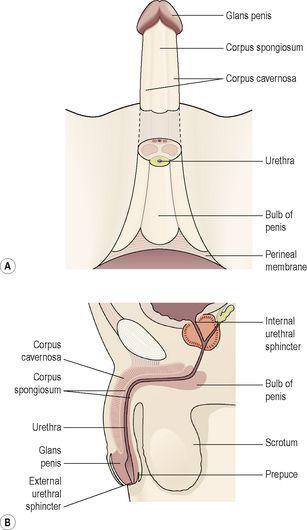
Urethra and penis
Urethra
The male urethra provides a common pathway for the flow of urine and semen, the combined secretions of the male reproductive organs. It is about 19 to 20 cm long and consists of three parts. The
prostatic urethra
originates at the urethral orifice of the bladder and passes through the prostate gland. The
membranous urethra
is the shortest and narrowest part and extends from the prostate gland to the bulb of the penis, after passing through the perineal membrane. The
spongiose
or
penile urethra
lies within the corpus spongiosum of the penis and terminates at the external urethral orifice in the
glans penis
.
There are two urethral sphincters (
Fig. 18.17
). The
internal sphincter
consists of smooth muscle fibres at the neck of the bladder above the prostate gland. The
external sphincter
consists of skeletal muscle fibres surrounding the membranous part.
Figure 18.17
The penis: A.
Viewed from below.
B.
Viewed from the side.
Penis