Ross & Wilson Anatomy and Physiology in Health and Illness (205 page)
Read Ross & Wilson Anatomy and Physiology in Health and Illness Online
Authors: Anne Waugh,Allison Grant
Tags: #Medical, #Nursing, #General, #Anatomy

Uterosacral ligaments
These originate from the posterior walls of the cervix and vagina and extend backwards, one on each side of the rectum, to the sacrum.
Transverse cervical (cardinal) ligaments
These extend one from each side of the cervix and vagina to the side walls of the pelvis.
Pubocervical fascia
This extends forward from the transverse cervical ligaments on each side of the bladder and is attached to the posterior surface of the pubic bones.
Functions of the uterus
After puberty, the endometrium of the uterus goes through a regular monthly cycle of changes, the
menstrual cycle
, under the control of hypothalamic and anterior pituitary hormones (see
Ch. 9
). The purpose of the menstrual cycle is to prepare the uterus to receive, nourish and protect a fertilised ovum. The cycle is usually regular, lasting between 26 and 30 days. If the ovum is not fertilised a new cycle begins with a short period of bleeding (menstruation).
If the ovum is fertilised the zygote embeds itself in the uterine wall. The uterine muscle grows to accommodate the developing baby, which is called an
embryo
during its first 8 weeks, and a
fetus
for the remainder of the pregnancy. Uterine secretions nourish the ovum before it implants in the endometrium, and after implantation the rapidly expanding ball of cells is nourished by the endometrial cells themselves. This is sufficient for only the first few weeks and the
placenta
is the organ that takes over thereafter (see
Ch. 5
). The placenta, which is attached to the fetus by the umbilical cord, is also firmly attached to the wall of the uterus, and provides the route by which the growing baby receives oxygen and nutrients, and gets rid of its wastes. During pregnancy, which normally lasts about 40 weeks, the muscular walls of the uterus are prevented from contracting and expelling the baby early by high levels of the hormone progesterone secreted by the placenta. At the end of pregnancy (at term) the hormone oestrogen, which increases uterine contractility, becomes the predominant sex hormone in the blood. Additionally, oxytocin is released from the posterior pituitary, and also stimulates contraction of the uterine muscle. Control of oxytocin release is by positive feedback (see also
Fig. 9.5, p. 212
). During labour, the uterus forcefully expels the baby by means of powerful rhythmical contractions.
Uterine tubes
The uterine (Fallopian) tubes (
Fig. 18.3
) are about 10 cm long and extend from the sides of the uterus between the body and the fundus. They lie in the upper free border of the broad ligament and their trumpet-shaped lateral ends penetrate the posterior wall, opening into the peritoneal cavity close to the ovaries. The end of each tube has fingerlike projections called
fimbriae
. The longest of these is the
ovarian fimbria
, which is in close association with the ovary.
Structure
The uterine tubes have an outer covering of peritoneum (broad ligament), a middle layer of smooth muscle and are lined with ciliated epithelium.
Blood supply, lymph drainage and nerve supply
These are as for the uterus.
Functions
The uterine tubes move the ovum from the ovary to the uterus by peristalsis and ciliary movement. The mucus secreted by the mucosa provides ideal conditions for movement of ova and spermatozoa. Fertilisation of the ovum usually takes place in the uterine tube, and the zygote is propelled into the uterus for implantation.
Ovaries
The ovaries (
Fig. 18.3
) are the female gonads (glands producing sex hormones and the ova), and they lie in a shallow fossa on the lateral walls of the pelvis. They are 2.5 to 3.5 cm long, 2 cm wide and 1 cm thick. Each is attached to the upper part of the uterus by the ovarian ligament and to the back of the broad ligament by a broad band of tissue, the
mesovarium
. Blood vessels and nerves pass to the ovary through the mesovarium (
Fig. 18.7
).
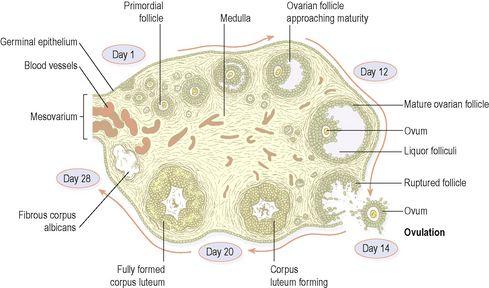
Figure 18.7
A section of an ovary showing the stages of development of one ovarian follicle.
Structure
The ovaries have two layers of tissue.
Medulla
This lies in the centre and consists of fibrous tissue, blood vessels and nerves.
Cortex
This surrounds the medulla. It has a framework of connective tissue, or
stroma
, covered by
germinal epithelium
. It contains
ovarian follicles
in various stages of maturity, each of which contains an ovum. Before puberty the ovaries are inactive but the stroma already contains immature (primordial) follicles, which the female has from birth. During the childbearing years, about every 28 days, one ovarian follicle (Graafian follicle) matures, ruptures and releases its ovum into the peritoneal cavity. This is called
ovulation
and it occurs during most menstrual cycles (
Figs 18.7
and
18.8
). Following ovulation, the ruptured follicle develops into the corpus luteum (meaning ‘yellow body’), which in turn will leave a small permanent scar of fibrous tissue called the corpus albicans (meaning ‘white body’) on the surface of the ovary.
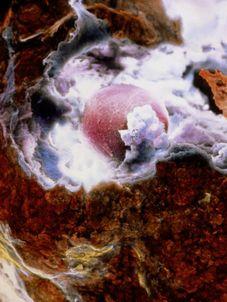
Figure 18.8
The moment of ovulation:
scanning electron micrograph of an ovum (pink) emerging through the surface of the ovary (brown).
Blood supply, lymph drainage and nerve supply
Arterial supply
This is by the ovarian arteries, which branch from the abdominal aorta just below the renal arteries.
Venous drainage
This is into a plexus of veins behind the uterus from which the ovarian veins arise. The right ovarian vein opens into the inferior vena cava and the left into the left renal vein.
Lymph drainage
This is to the lateral aortic and preaortic lymph nodes. The lymph vessels follow the same route as the arteries.
Nerve supply
The ovaries are supplied by parasympathetic nerves from the sacral outflow and sympathetic nerves from the lumbar outflow.
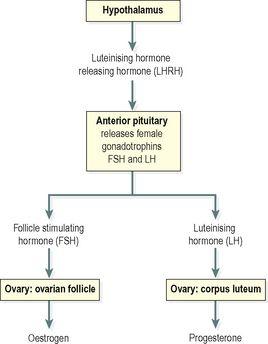
Functions
The ovary is the organ in which the female gametes are stored and develop prior to ovulation. Their maturation is controlled by the hypothalamus and the anterior pituitary gland, which releases gonadotrophins (follicle stimulating hormone, FSH, and luteinising hormone, LH), both of which act on the ovary. In addition, the ovary has endocrine functions, and releases hormones essential to the physiological changes during the reproductive cycle. The source of these hormones, oestrogen and progesterone, is the follicle itself. During the first half of the cycle, while the ovum is developing within the follicle, the follicle secretes increasing amounts of oestrogen. However, after ovulation, the corpus luteum secretes primarily progesterone, with some oestrogen (
Fig 18.9
). The significance of this is discussed under the menstrual cycle (see below).
Figure 18.9
Female reproductive hormones and target tissues.
Puberty in the female
Puberty is the age at which the internal reproductive organs reach maturity, usually between the ages of 12 and 14. This is called the menarche, and marks the beginning of the childbearing period. The ovaries are stimulated by the gonadotrophins from the anterior pituitary: follicle stimulating hormone and luteinising hormone.
A number of physical and psychological changes take place at puberty:
•
the uterus, the uterine tubes and the ovaries reach maturity
•
the menstrual cycle and ovulation begin (menarche)
•
the breasts develop and enlarge
•
pubic and axillary hair begins to grow
•
increase in height and widening of the pelvis
•
increased fat deposited in the subcutaneous tissue, especially at the hips and breasts.
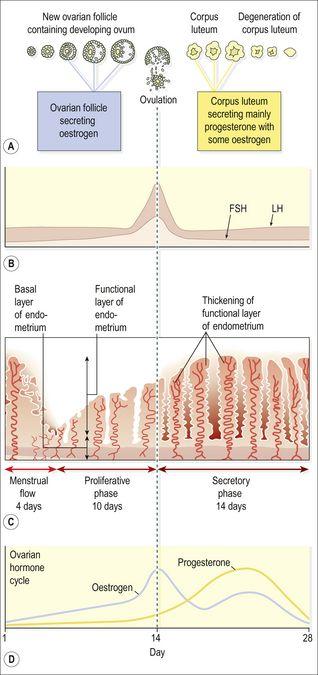
The reproductive cycle
This is a series of events, occurring regularly in females every 26 to 30 days throughout the childbearing period of about 36 years (
Fig. 18.10
). The cycle consists of a series of changes taking place concurrently in the ovaries and uterine walls, stimulated by changes in blood concentrations of hormones (
Fig. 18.10B and D
). Hormones secreted during the cycle are regulated by negative feedback mechanisms.
Figure 18.10
Summary of one female reproductive cycle: A.
Ovarian cycle; maturation of follicle and development of corpus luteum.
B.
Anterior pituitary cycle; LH and FSH levels.
C.
Uterine cycle; menstrual, proliferative and secretory phases.
D.
Ovarian hormone cycle; oestrogen and progesterone levels.