Ross & Wilson Anatomy and Physiology in Health and Illness (204 page)
Read Ross & Wilson Anatomy and Physiology in Health and Illness Online
Authors: Anne Waugh,Allison Grant
Tags: #Medical, #Nursing, #General, #Anatomy

The vestibular glands (Bartholin’s glands) are situated one on each side near the vaginal opening. They are about the size of a small pea and have ducts, opening into the vestibule immediately lateral to the attachment of the hymen. They secrete mucus that keeps the vulva moist.
Blood supply, lymph drainage and nerve supply
Arterial supply
This is by branches from the internal pudendal arteries that branch from the internal iliac arteries and by external pudendal arteries that branch from the femoral arteries.
Venous drainage
This forms a large plexus which eventually drains into the internal iliac veins.
Lymph drainage
This is through the superficial inguinal nodes.
Nerve supply
This is by branches from pudendal nerves.
Perineum
The perineum is the area extending from the base of the labia minora to the anal canal. It is roughly triangular and consists of connective tissue, muscle and fat. It gives attachment to the muscles of the pelvic floor (
p. 416
).
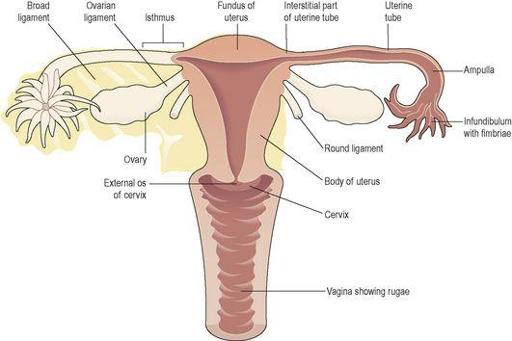
Internal genitalia
The internal organs of the female reproductive system (
Figs 18.3
and
18.4
) lie in the pelvic cavity and consist of the vagina, uterus, two uterine tubes and two ovaries.
Figure 18.3
The female reproductive organs in the pelvis.
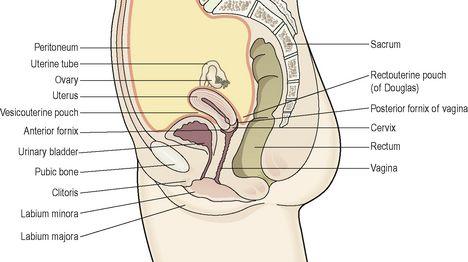
Figure 18.4
Lateral view of the female reproductive organs in the pelvis and their associated structures.
Vagina
The vagina is a fibromuscular tube lined with stratified squamous epithelium (
Fig. 3.14, p. 35
), connecting the external and internal organs of reproduction. It runs obliquely upwards and backwards at an angle of about 45° between the bladder in front and rectum and anus behind. In the adult, the anterior wall is about 7.5 cm long and the posterior wall about 9 cm long. The difference is due to the angle of insertion of the cervix through the anterior wall.
Structure of the vagina
The vagina has three layers: an outer covering of areolar tissue, a middle layer of smooth muscle and an inner lining of stratified squamous epithelium that forms ridges or
rugae
. It has no secretory glands but the surface is kept moist by cervical secretions. Between puberty and the menopause,
Lactobacillus acidophilus
bacteria are normally present, which secrete lactic acid, maintaining the pH between 4.9 and 3.5. The acidity inhibits the growth of most other micro-organisms that may enter the vagina from the perineum.
Blood supply, lymph drainage and nerve supply
Arterial supply
An arterial plexus is formed round the vagina, derived from the uterine and vaginal arteries, which are branches of the internal iliac arteries.
Venous drainage
A venous plexus, situated in the muscular wall, drains into the internal iliac veins.
Lymph drainage
This is through the deep and superficial iliac glands.
Nerve supply
This consists of parasympathetic fibres from the sacral outflow, sympathetic fibres from the lumbar outflow and somatic sensory fibres from the pudendal nerves.
Functions of the vagina
The vagina acts as the receptacle for the penis during sexual intercourse (coitus), and provides an elastic passageway through which the baby passes during childbirth.
Uterus
The uterus is a hollow muscular pear-shaped organ, flattened anteroposteriorly. It lies in the pelvic cavity between the urinary bladder and the rectum (
Fig. 18.4
).
In most women, it leans forward (
anteversion
), and is bent forward (
anteflexion
) almost at right angles to the vagina, so that its anterior wall rests partly against the bladder below, and forming the vesicouterine pouch between the two organs.
When the body is upright, the uterus lies in an almost horizontal position. It is about 7.5 cm long, 5 cm wide and its walls are about 2.5 cm thick. It weighs from 30 to 40 grams. The parts of the uterus are the fundus, body and cervix (
Fig. 18.3
).
Fundus
This is the dome-shaped part of the uterus above the openings of the uterine tubes.
Body
This is the main part. It is narrowest inferiorly at the
internal os
where it is continuous with the cervix.
Cervix (‘neck’ of the uterus)
This protrudes through the anterior wall of the vagina, opening into it at the
external os
.
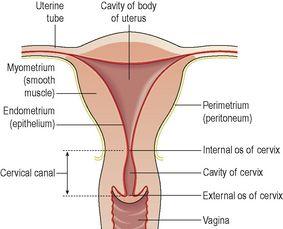
Structure
The walls of the uterus are composed of three layers of tissue: perimetrium, myometrium and endometrium (
Fig. 18.5
).
Figure 18.5
A section of the uterus.
Perimetrium
This is peritoneum, which is distributed differently on the various surfaces of the uterus (
Fig. 18.4
).
Anteriorly it lies over the fundus and the body where it is folded on to the upper surface of the urinary bladder. This fold of peritoneum forms the
vesicouterine pouch
.
Posteriorly the peritoneum covers the fundus, the body and the cervix, then it folds back on to the rectum to form the
rectouterine pouch
(of Douglas).
Laterally, only the fundus is covered because the peritoneum forms a double fold with the uterine tubes in the upper free border. This double fold is the
broad ligament
, which, at its lateral ends, attaches the uterus to the sides of the pelvis.
Myometrium
This is the thickest layer of tissue in the uterine wall. It is a mass of smooth muscle fibres interlaced with areolar tissue, blood vessels and nerves.
Endometrium
This consists of columnar epithelium containing a large number of mucus-secreting tubular glands. It is divided functionally into two layers:
•
The
functional layer
is the upper layer and it thickens and becomes rich in blood vessels in the first half of the menstrual cycle. If the ovum is not fertilised and does not implant, this layer is shed during menstruation.
•
The
basal layer
lies next to the myometrium, and is not lost during menstruation. It is the layer from which the fresh functional layer is regenerated during each cycle.
The upper two-thirds of the cervical canal is lined with this mucous membrane. Lower down, however, the mucosa changes, becoming stratified squamous epithelium, which is continuous with the lining of the vagina itself.
Blood supply, lymph drainage and nerve supply
Arterial supply
This is by the uterine arteries, branches of the internal iliac arteries. They pass up the lateral aspects of the uterus between the two layers of the broad ligaments. They supply the uterus and uterine tubes and join with the ovarian arteries to supply the ovaries.
Venous drainage
The veins follow the same route as the arteries and eventually drain into the internal iliac veins.
Lymph drainage
Deep and superficial lymph vessels drain lymph from the uterus and the uterine tubes to the aortic lymph nodes and groups of nodes associated with the iliac blood vessels.
Nerve supply
The nerves supplying the uterus and the uterine tubes consist of parasympathetic fibres from the sacral outflow and sympathetic fibres from the lumbar outflow.
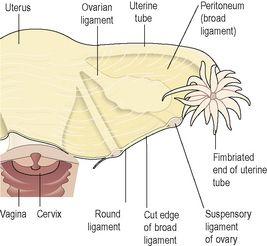
Supporting structures
The uterus is supported in the pelvic cavity by surrounding organs, muscles of the pelvic floor and ligaments that suspend it from the walls of the pelvis (
Fig. 18.6
).
Figure 18.6
The main ligaments supporting the uterus.
Only one side is shown.
Broad ligaments
These are formed by a double fold of peritoneum, one on each side of the uterus. They hang down from the uterine tubes as though draped over them and at their lateral ends they are attached to the sides of the pelvis. The uterine tubes are enclosed in the upper free border and near the lateral ends they penetrate the posterior wall of the broad ligament and open into the peritoneal cavity. The ovaries are attached to the posterior wall, one on each side. Blood and lymph vessels and nerves pass to the uterus and uterine tubes between the layers of the broad ligaments.
Round ligaments
These are bands of fibrous tissue between the two layers of broad ligament, one on each side of the uterus. They pass to the sides of the pelvis then through the
inguinal canal
to end by fusing with the labia majora.