Ross & Wilson Anatomy and Physiology in Health and Illness (142 page)
Read Ross & Wilson Anatomy and Physiology in Health and Illness Online
Authors: Anne Waugh,Allison Grant
Tags: #Medical, #Nursing, #General, #Anatomy

The
hepatic artery
enters, carrying arterial blood. It is a branch from the coeliac artery, which is a branch from the abdominal aorta.
Nerve fibres
, sympathetic and parasympathetic, enter here.
The
right
and
left hepatic ducts
leave, carrying bile from the liver to the gall bladder.
Lymph vessels
leave the liver, draining some lymph to abdominal and some to thoracic nodes.
Blood supply (see
Figs 5.44
and
5.46
)
The hepatic artery and the portal vein take blood to the liver (see
Fig. 12.36
). Venous return is by a variable number of hepatic veins that leave the posterior surface and immediately enter the inferior vena cava just below the diaphragm.
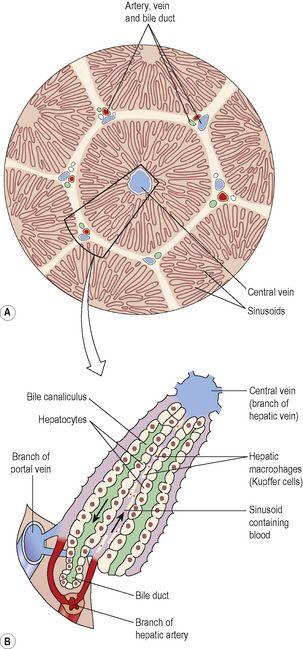
Structure
The lobes of the liver are made up of tiny functional units, called
lobules
, which are just visible to the naked eye (
Fig. 12.35A
). Liver lobules are hexagonal in outline and are formed by cubical-shaped cells, the
hepatocytes
, arranged in pairs of columns radiating from a central vein. Between two pairs of columns of cells are
sinusoids
(blood vessels with incomplete walls,
Ch. 5
) containing a mixture of blood from the tiny branches of the portal vein and hepatic artery (
Fig. 12.35B
). This arrangement allows the arterial blood and portal venous blood (with a high concentration of nutrients) to mix and come into close contact with the liver cells. Amongst the cells lining the sinusoids are hepatic macrophages (Kupffer cells) whose function is to ingest and destroy worn out blood cells and any foreign particles present in the blood flowing through the liver.
Figure 12.35
A.
A magnified transverse section of a liver lobule.
B.
Direction of the flow of blood and bile in a liver lobule.
Blood drains from the sinusoids into
central
or
centrilobular veins
. These then join with veins from other lobules, forming larger veins, until eventually they become the hepatic veins, which leave the liver and empty into the inferior vena cava.
Figure 12.36
shows the system of blood flow through the liver. One of the functions of the liver is to secrete
bile
. In
Figure 12.35B
it is seen that
bile canaliculi
run between the columns of liver cells. This means that each column of hepatocytes has a blood sinusoid on one side and a bile canaliculus on the other. The canaliculi join up to form larger bile canals until eventually they form the
right and left hepatic ducts
, which drain bile from the liver.
Lymphoid tissue and a system of lymph vessels are also present in each lobule.
Functions of the liver
The liver is an extremely active organ. Those functions already described are only mentioned here.
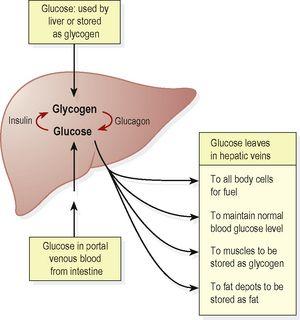
Carbohydrate metabolism
The liver has an important role in maintaining plasma glucose levels. After a meal when levels rise, glucose is converted to glycogen for storage under the influence of the hormone insulin. Later, when glucose levels fall, the hormone glucagon stimulates conversion of glycogen into glucose again, keeping levels within the normal range (see
Fig 12.39
).
Figure 12.39
Summary of the source, distribution and use of glucose.
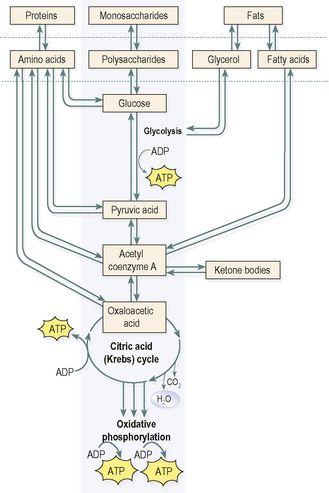
Fat metabolism
Stored fat can be converted to a form in which it can be used by the tissues to provide energy (see
Fig. 12.44
).
Figure 12.44
Summary of the fates of the three main energy sources in the central metabolic pathways.
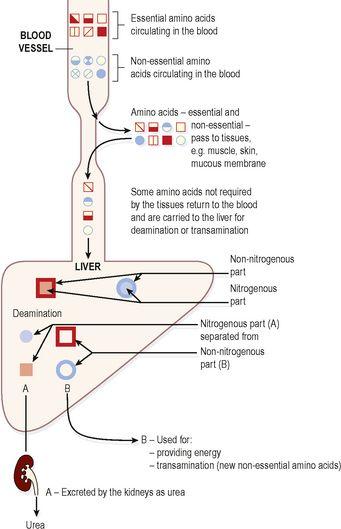
Protein metabolism
Deamination of amino acids
This process:
•
removes the nitrogenous portion from the amino acids not required for the formation of new protein;
urea
is formed from this nitrogenous portion which is excreted in urine
•
breaks down nucleic acids (genetic material, see
p. 24
and
Ch. 17
) to form
uric acid
, which is excreted in the urine.
Transamination
Removes the nitrogenous portion of amino acids and attaches it to other carbohydrate molecules forming new non-essential amino acids (see
Fig. 12.42
).
Figure 12.42
The fate of amino acids in the body.
Synthesis of plasma proteins
and most blood clotting factors from amino acids.
Breakdown of erythrocytes and defence against microbes
This is carried out by phagocytic hepatic macrophages (Kupffer cells) in the sinusoids (breakdown of red blood cells also takes place in the spleen and bone marrow).
Detoxification of drugs and toxic substances
These include ethanol (alcohol) and toxins produced by, e.g., microbes. Some drugs are extensively inactivated by the liver and are not very effective when given by mouth (orally), e.g. glyceryl trinitrate. This is because after absorption from the alimentary tract, they travel in the blood to the liver where they are largely metabolised so that levels in the blood leaving the liver are inadequate to achieve therapeutic effects. This is known as ‘
first pass metabolism’
.
Inactivation of hormones
These include insulin, glucagon, cortisol, aldosterone, thyroid and sex hormones.
Production of heat
The liver uses a considerable amount of energy, has a high metabolic rate and produces a great deal of heat. It is the main heat-producing organ of the body.
Secretion of bile
The hepatocytes synthesise the constituents of bile from the mixed arterial and venous blood in the sinusoids. These include bile salts, bile pigments and cholesterol.
Storage
Stored substances include:
•
glycogen (see
p. 307
)
•
fat-soluble vitamins: A, D, E, K
•
iron, copper
•
some water-soluble vitamins, e.g. vitamin B
12
.
Composition of bile
Between 500 and 1000 ml of bile are secreted by the liver daily. Bile consists of:
•
water
•
mineral salts
•
mucus
•
bile pigments, mainly bilirubin
•
bile salts, which are derived from the primary bile acids, cholic acid and chenodeoxycholic acid
•
cholesterol.
The bile acids,
cholic
and
chenodeoxycholic acid
, are synthesised by hepatocytes from cholesterol, then secreted into bile as sodium or potassium salts. In the small intestine they emulsify fats, aiding their digestion. In the terminal ileum most of the bile salts are reabsorbed and return to the liver in the portal vein. This
enterohepatic circulation
, or recycling of bile salts, ensures that large amounts of bile salts enter the small intestine daily from a relatively small bile acid pool (
Fig. 12.37
).
Bilirubin
is one of the products of haemolysis of erythrocytes by hepatic macrophages (Kupffer cells) in the liver and by other macrophages in the spleen and bone marrow. Bilirubin is insoluble in water and is carried in the blood bound to albumin. In hepatocytes it is
conjugated
(combined) with glucuronic acid and becomes water-soluble enough to be excreted in bile. Bacteria in the intestine change the form of bilirubin and most is excreted as
stercobilin
in the faeces. A small amount is reabsorbed and excreted in urine as
urobilinogen
(
Fig. 12.37
). Jaundice is yellow pigmentation of the tissues, seen in the skin and conjunctiva, caused by excess blood bilirubin (
p. 326
).
Biliary tract
Learning outcomes
After studying this section, you should be able to:
describe the route taken by bile from the liver, to the gall bladder, and then to the duodenum