Ross & Wilson Anatomy and Physiology in Health and Illness (143 page)
Read Ross & Wilson Anatomy and Physiology in Health and Illness Online
Authors: Anne Waugh,Allison Grant
Tags: #Medical, #Nursing, #General, #Anatomy

outline the structure and functions of the gall bladder.
Bile ducts (
Fig. 12.38
)
The
right
and
left hepatic ducts
join to form the
common hepatic duct
just outside the portal fissure. The hepatic duct passes downwards for about 3 cm where it is joined by the
cystic duct
from the gall bladder. The cystic and hepatic ducts merge forming the
common bile duct
, which passes downwards behind the head of the pancreas. This is joined by the main pancreatic duct at the hepatopancreatic ampulla and the opening into the duodenum, at the duodenal papilla, is controlled by the hepatopancreatic sphincter (of Oddi). The common bile duct is about 7.5 cm long and has a diameter of about 6 mm.
Structure
The walls of the bile ducts have the same layers of tissue as those described in the basic structure of the alimentary canal (
Fig. 12.2
). In the cystic duct the mucous membrane lining is arranged in irregular circular folds, which have the effect of a spiral valve. Bile passes through the cystic duct twice – once on its way into the gall bladder and again when it is expelled from the gall bladder into the common bile duct and then on to the duodenum.
Gall bladder
The gall bladder is a pear-shaped sac attached to the posterior surface of the liver by connective tissue. It has a
fundus
or expanded end, a
body
or main part and a
neck
, which is continuous with the cystic duct.
Structure
The wall of the gall bladder has the same layers of tissue as those described in the basic structure of the alimentary canal, with some modifications.
Peritoneum
This covers only the inferior surface because the upper surface of the gall bladder is in direct contact with the liver and held in place by the visceral peritoneum that covers the liver.
Muscle layer
There is an additional layer of oblique muscle fibres.
Mucous membrane
This displays small rugae when the gall bladder is empty that disappear when it is distended with bile.
Blood supply
The
cystic artery
, a branch of the hepatic artery, supplies blood to the gall bladder. Blood is drained away by the
cystic vein
that joins the portal vein.
Functions of the gall bladder
These include:
•
reservoir for bile
•
concentration of the bile by up to 10- or 15-fold, by absorption of water through the walls of the gall bladder
•
release of stored bile.
When the muscle wall of the gall bladder contracts, bile passes through the bile ducts to the duodenum. Contraction is stimulated by:
•
the hormone cholecystokinin (CCK), secreted by the duodenum
•
the presence of fat and acid chyme in the duodenum.
Relaxation of the hepatopancreatic sphincter (of Oddi) is caused by CCK and is a reflex response to contraction of the gall bladder.
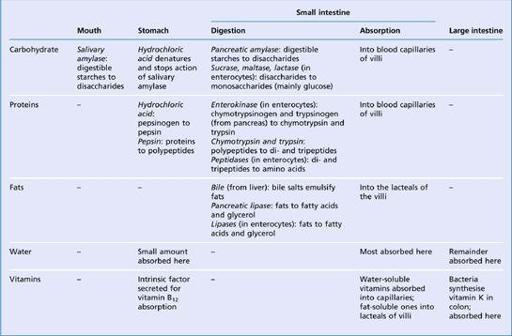
Summary of digestion and absorption of nutrients
Learning outcomes
After studying this section, you should be able to:
list the principal digestive enzymes, their sites of action, their substrates and their products
describe the sites of absorption of the main nutrient groups.
Table 12.2
summarises the main digestive processes of the principal nutrient groups, the locations where these processes occur and the enzymes involved.
Table 12.2
Summary showing the sites of digestion and absorption of nutrients
Metabolism
Learning outcomes
After studying this section, you should be able to:
discuss general principles of metabolism, including anabolism, catabolism, units of energy and metabolic rate