Ross & Wilson Anatomy and Physiology in Health and Illness (82 page)
Read Ross & Wilson Anatomy and Physiology in Health and Illness Online
Authors: Anne Waugh,Allison Grant
Tags: #Medical, #Nursing, #General, #Anatomy

These diseases are caused either by injury to axons or by disorders of cells that secrete myelin, i.e. oligodendrocytes and Schwann cells.
Multiple sclerosis (MS)
In this disease there are areas of demyelinated white matter, called plaques, irregularly distributed throughout the brain and spinal cord. Grey matter in the brain and spinal cord may also be affected because of the arrangement of satellite oligodendrocytes round cell bodies. In the early stages there may be little damage to axons.
It usually develops between the ages of 20 and 40 years and affects twice as many women as men. The actual cause(s) of MS are not known but several factors seem to be involved. It appears to be an autoimmune disorder, possibly triggered by a viral infection, e.g. measles.
Environment before adolescence
is implicated because the disease is most prevalent in people who spend their preadolescent years in temperate climates, and those who move to other climates after that age retain their susceptibility to MS. People from equatorial areas moving into a temperate climate during adolescence or later life appear not to be susceptible.
Genetic factors
are implicated too as there is an increased incidence of MS among siblings, especially identical twins, and parents of patients.
Effects of multiple sclerosis
Damage leads to a variety of consequences, depending on the sites and sizes of demyelinated plaques, which damage white matter. This results in upper motor neurone dysfunction causing:
•
weakness of skeletal muscles and sometimes paralysis
•
lack of coordination and movement
•
disturbed sensation, e.g. burning or pins and needles
•
incontinence of urine
•
visual disturbances, especially blurring and double vision. The optic nerves are commonly affected early in the disease.
The disease pattern is usually one of relapses and remissions of widely varying duration. Each relapse causes further loss of nervous tissue and progressive dysfunction. In some cases there may be chronic progression without remission, or acute disease rapidly leading to death.
Acute disseminated encephalomyelitis
This is a rare but serious condition that may occur:
•
as a complication of a viral infection, e.g. measles, chickenpox
•
following primary immunisation against viral diseases, mainly in older children and adults.
The cause of the acute diffuse demyelination is not known. It has been suggested that an autoimmune effect on myelin is triggered either by viruses during a viral infection such as measles, or by an immune response to vaccines. The effects vary considerably, according to the distribution and degree of demyelination and are similar to those of MS. The early febrile state may progress to paralysis and coma. Most patients survive the initial phase and recover completely but some have severe neurological impairment.
Diseases of the spinal cord
Learning outcome
After studying this section you should be able to:
explain how disorders of the spinal cord cause abnormal function.
Because space in the neural canal and intervertebral foramina is limited, any condition that distorts their shape or reduces the space may damage the spinal cord or peripheral nerve roots, or cause ischaemia by compressing blood vessels. Such conditions include:
•
fracture and/or dislocation of vertebrae
•
tumours of the meninges or vertebrae
•
prolapsed intervertebral disc.
The effects of disease or injury depend on the severity of the damage, the type and position of the neurones involved, i.e. motor, sensory, proprioceptor, autonomic, connector neurones in reflex arcs in the spinal cord or in peripheral nerves.
Motor neurones
Table 7.4
gives a summary of the effects of damage to the motor neurones. The parts of the body affected depend on which neurones have been damaged and their site in the brain, spinal cord or peripheral nerve.
Table 7.4
Summary of effects of damage to motor neurones
| Upper motor neurone | Lower motor neurone |
|---|---|
| Muscle weakness and spastic paralysis | Muscle weakness and flaccid paralysis |
| Exaggerated tendon reflexes | Absence of tendon reflexes |
| Muscle twitching | Muscle wasting Contracture of muscles Impaired circulation |
Upper motor neurone (UMN) lesions
Lesions of the UMNs above the level of the decussation of the pyramids affect the opposite side of the body, e.g. haemorrhage or infarction in the internal capsule of one hemisphere causes paralysis of the opposite side of the body. Lesions below the decussation affect the same side of the body. The lower motor neurones are released from cortical control and muscle tone is increased (
Table 7.4
).
Lower motor neurone (LMN) lesions
The cell bodies of LMNs are in the spinal cord and the axons are part of peripheral nerves. Lesions of LMNs lead to weakness or paralysis of the effector muscles they supply.
Motor neurone disease
This is a chronic progressive degeneration of upper and lower motor neurones, occurring more commonly in men over 50 years of age. The cause is seldom known, although a few cases are inherited as an autosomal dominant disorder (
p. 433
). Motor neurones in the cerebral cortex, brain stem and anterior horns of the spinal cord are destroyed and replaced by gliosis. Early effects are usually weakness and twitching of the small muscles of the hand, and muscles of the arm and shoulder girdle. The legs are affected later. Death occurs within 3–5 years and is usually due to respiratory difficulties or complications of immobility.
Sensory neurones
The sensory functions lost as a result of disease or injury depend on which neurones have been damaged. Spinal cord damage leads to loss of sensation and cerebellar function. Peripheral nerve damage leads to loss of reflex activity, loss of sensation and of cerebellar function.
Mixed motor and sensory conditions
Subacute combined degeneration of the spinal cord
This condition most commonly occurs as a complication of pernicious anaemia (
p. 67
). Vitamin B
12
is needed for the formation and maintenance of myelin by Schwann cells and oligodendrocytes. Although degeneration of the spinal cord may be apparent before the anaemia, it is arrested by treatment with vitamin B
12
.
The degeneration of myelin occurs in the posterior and lateral columns of white matter in the spinal cord, especially in the upper thoracic and lower cervical regions. Less frequently the changes occur in the posterior root ganglia and peripheral nerves. Demyelination of proprioceptor fibres (sensory) leads to ataxia and involvement of upper motor neurones leads to increased muscle tone and spastic paralysis. Without treatment, death may occur within 5 years.
Compression of the spinal cord and nerve roots
The causes include:
•
prolapsed intervertebral disc
•
syringomyelia
•
tumours: metastatic, meningeal or nerve sheath
•
fractures with displacement of bone fragments.
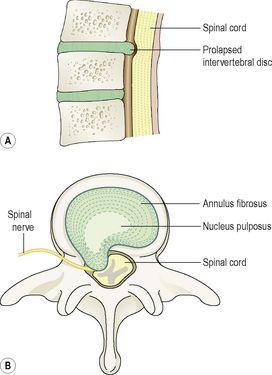
Prolapsed intervertebral disc (
Fig. 7.52
)
This is the most common cause of compression of the spinal cord and/or nerve roots. The vertebral bodies are separated by the intervertebral discs, each consisting of an outer rim of cartilage, the
annulus fibrosus
, and a central core of soft gelatinous material, the
nucleus pulposus
.
Figure 7.52
Prolapsed intervertebral disc. A.
Viewed from the side.
B.
Viewed from above.
Prolapse of a disc is herniation of the nucleus pulposus, causing the annulus fibrosus and the posterior longitudinal ligament to protrude into the neural canal. It is most common in the lumbar region, usually below the level of the spinal cord, i.e. below L2, and therefore affects nerve roots only. If it occurs in the cervical region, the cord may also be compressed. Herniation may occur suddenly, typically in young adults during strenuous exercise or exertion, or progressively in older people when bone disease or degeneration of the disc leads to rupture during minimal exercise. The hernia may be: