Ross & Wilson Anatomy and Physiology in Health and Illness (168 page)
Read Ross & Wilson Anatomy and Physiology in Health and Illness Online
Authors: Anne Waugh,Allison Grant
Tags: #Medical, #Nursing, #General, #Anatomy

Figure 14.5
The nail and related skin.
The
root
of the nail is embedded in the skin and covered by the cuticle, which forms the hemispherical pale area called the
lunula
.
The
nail plate
is the exposed part that has grown out from the germinative zone of the epidermis called the
nail bed
.
Finger nails grow more quickly than toe nails and growth is quicker when the environmental temperature is high.
Functions of the skin
Protection
The skin forms a relatively waterproof layer, provided mainly by its keratinised epithelium, which protects the deeper and more delicate structures. As an important non-specific defence mechanism it acts as a barrier against:
•
invasion by micro-organisms
•
chemicals
•
physical agents, e.g. mild trauma, ultraviolet light
•
dehydration.
The epidermis contains specialised immune cells called Langerhans cells, which are a type of microphage. They phagocytose intruding antigens and travel to lymphoid tissue, where they present antigen to T-lymphocytes, thus stimulating an immune response (
p. 370
).
Due to the presence of the sensory nerve endings in the skin the body reacts by reflex action (withdrawal) to unpleasant or painful stimuli, protecting it from further injury (
p. 158
).
The pigment melanin affords some protection against harmful ultraviolet rays in sunlight.
Regulation of body temperature
Body temperature remains fairly constant at about 36.8°C across a wide range of environmental temperatures ensuring that the optimal range for enzyme activity required for metabolism is maintained. In health, variations are usually limited to between 0.5 and 0.75°C, although it rises slightly in the evening, during exercise and in women just after ovulation. To ensure this constant temperature, a negative feedback system maintains the balance between heat produced in the body and heat lost to the environment.
Heat production
When metabolic rate increases, body temperature rises, and when it decreases body temperature falls. Some of the energy released during metabolic activity is in the form of heat and the most active organs produce most heat. The principal organs involved are:
•
skeletal muscles
– contraction of skeletal muscles produces a large amount of heat and the more strenuous the muscular exercise, the greater the heat produced. Shivering also involves skeletal muscle contraction, which increases heat production when there is the risk of the body temperature falling below normal.
•
the liver
is very metabolically active, and heat is produced as a by-product. Metabolic rate and heat production are increased after eating.
•
the digestive organs
produce heat during peristalsis and during the chemical reactions involved in digestion.
Heat loss
Most heat loss from the body occurs through the skin. Small amounts are lost in expired air, urine and faeces. Only heat loss through the skin can be regulated; heat lost by the other routes cannot be controlled.
Heat loss through the skin is affected by the difference between body and environmental temperatures, the amount of the body surface exposed and the type of clothes worn. Air insulates against heat loss when trapped in layers of clothing and between the skin and clothing. For this reason several layers of lightweight clothes provide more effective insulation against low environmental temperatures than one heavy garment.
Mechanisms of heat loss
In
evaporation
, the body is cooled as heat converts the water in sweat to water vapour. In
radiation
, exposed parts of the body radiate heat away from the body. In
conduction
, clothes and other objects in direct contact with the skin take up heat. In
convection
, air passing over the exposed parts of the body is heated and rises, cool air replaces it and convection currents are set up. Convection also cools the body when clothes are worn, except when they are windproof.
Control of body temperature
The
temperature regulating centre
in the hypothalamus is sensitive to the temperature of circulating blood. This centre responds to decreasing temperature by sending nerve impulses to:
•
arterioles in the dermis, which constrict decreasing blood flow to the skin
•
skeletal muscles stimulating shivering.
As heat is conserved, body temperature rises and when it returns to the normal range again the negative feedback mechanism is switched off (see
Fig. 1.15, p. 7
)
Conversely when body temperature rises, heat loss is increased by dilation of arterioles in the dermis, increasing blood flow to the skin, and stimulation of the sweat glands causing sweating, until it falls into the normal range again when the negative feedback mechanism is switched off.
Activity of the sweat glands
When body temperature is increased by 0.25 to 0.5°C the sweat glands secrete sweat onto the skin surface. Evaporation of sweat cools the body, but is slower in humid conditions.
Loss of heat from the body by evaporation of water through the skin and expired air still occurs even when the environmental temperature is low. This is called
insensible water loss
(around 500 ml per day) and is accompanied by insensible heat loss.
Regulation of blood flow through the skin
The amount of heat lost from the skin depends largely on blood flow through dermal capillaries. As body temperature rises, the arterioles dilate and more blood enters the capillary network in the skin. The skin is warm and pink in colour. In addition to increasing the amount of sweat produced, the temperature of the skin rises and more heat is lost by radiation, conduction and convection.
If the environmental temperature is low or if heat production is decreased, the arterioles in the dermis are constricted. This reduces the blood flow near the body surface, conserving heat. The skin appears paler and feels cool.
Fever
This is often the result of infection and is caused by release of chemicals (
pyrogens
) from inflammatory cells and invading bacteria. Pyrogens act on the hypothalamus, which releases prostaglandins that reset the hypothalamic thermostat to a higher temperature. The body responds by activating heat-promoting mechanisms, e.g. shivering and vasoconstriction, until the new higher temperature is reached. When the thermostat is reset to the normal level, heat-loss mechanisms are activated. There is profuse sweating and vasodilation accompanied by warm, pink (flushed) skin until body temperature falls to the normal range again.
Hypothermia
This means a core (e.g. rectal) temperature below 35°C. At a core temperature below 32°C, compensatory mechanisms to restore body temperature usually fail, e.g. shivering is replaced by muscle rigidity and cramps, vasoconstriction fails and blood pressure, pulse and respiration rates fall. Mental confusion and disorientation occur. Death usually occurs when the temperature falls below 25°C.
Individuals at the extremes of age are prone to hypothermia as temperature regulation is less effective in the young and elderly.
Formation of vitamin D
7-dehydrocholesterol
is a lipid-based substance in the skin, and ultraviolet rays in sunlight convert it to vitamin D. This circulates in the blood and is used, with calcium and phosphate, in the formation and maintenance of bone.
Cutaneous sensation
Sensory receptors are nerve endings in the dermis that are sensitive to touch, pressure, temperature or pain. Stimulation generates nerve impulses in sensory nerves that are transmitted to the cerebral cortex (see
Fig. 7.23, p. 151
). Some areas have more sensory receptors than others causing them to be especially sensitive, e.g. the lips and fingertips.
Absorption
This property is limited but substances that can be absorbed include:
•
some drugs, in transdermal patches, e.g. hormone replacement therapy during the menopause, nicotine as an aid to stopping smoking
•
some toxic chemicals, e.g. mercury.
Excretion
The skin is a minor excretory organ for some substances including:
•
sodium chloride in sweat; excess sweating may lead to low blood sodium levels (hyponatraemia)
•
urea, especially when kidney function is impaired
•
aromatic substances, e.g. garlic and other spices.
Wound healing
Conditions required for wound healing
Systemic factors
These include good nutritional status and general health. Infection, impaired immunity, poor blood supply and systemic conditions, e.g. diabetes mellitus and cancer, reduce the rate of wound healing.
Local factors
Local factors that facilitate wound healing include a good blood supply to provide oxygen and nutrients and remove waste products, and freedom from contamination by, e.g., microbes, foreign bodies or toxic chemicals.
Primary healing (healing by first intention)
This method of healing follows minimal destruction of tissue when the damaged edges of a wound are in close apposition (
Fig. 14.6
). There are several overlapping stages in the repair process.
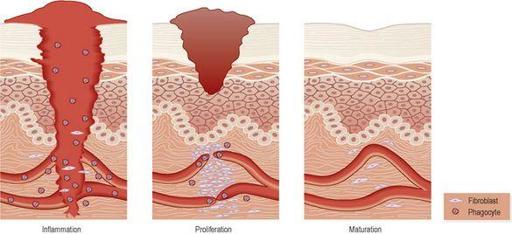
Figure 14.6
Stages in primary wound healing.
Inflammation
The cut surfaces become inflamed and blood clot and cell debris fill the gap between them in the first few hours. Phagocytes, including macrophages, and fibroblasts migrate into the blood clot:
•
phagocytes begin to remove the clot and cell debris, stimulating fibroblast activity
•
fibroblasts secrete collagen fibres which begin to bind the surfaces together.
Proliferation
Epithelial cells proliferate across the wound, through the clot. The epidermis meets and grows upwards until full thickness is restored. The clot above the new tissue becomes the scab and separates after 3 to 10 days.
Granulation tissue
, consisting of new capillary buds, phagocytes and fibroblasts, develops, invading the clot and restoring the blood supply to the wound. Fibroblasts continue to secrete collagen fibres as the clot and any bacteria are removed by phagocytosis.
Maturation
The granulation tissue is replaced by fibrous scar tissue. Rearrangement of collagen fibres occurs and the strength of the wound increases. In time the scar becomes less vascular, appearing after a few months as a fine line.
The channels left when stitches are removed heal by the same process.
Secondary healing (healing by second intention)
This method of healing follows destruction of a large amount of tissue or when the edges of a wound cannot be brought into apposition, e.g. varicose ulcers and pressure (decubitus) ulcers (
Fig. 14.7
). The stages of secondary healing are the same as in primary healing (see below) and the time taken for healing depends on the effective removal of the cause and the size of the wound.
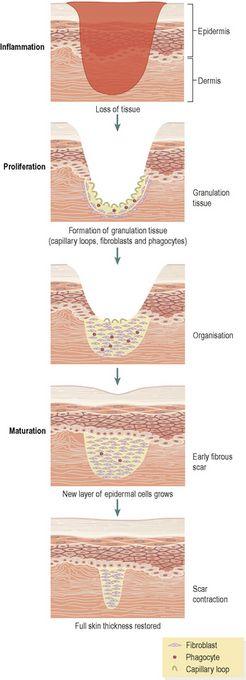
Figure 14.7
Stages in secondary wound healing.
Inflammation
This develops on the surface of the healthy tissue and separation of necrotic tissue (
slough
) begins, due mainly to the action of phagocytes in the inflammatory exudate. The inflammatory process is described on
page 367
.