Ross & Wilson Anatomy and Physiology in Health and Illness (172 page)
Read Ross & Wilson Anatomy and Physiology in Health and Illness Online
Authors: Anne Waugh,Allison Grant
Tags: #Medical, #Nursing, #General, #Anatomy

Complement is a system of about 20 proteins found in the blood and tissues. It is activated by the presence of immune complexes (an antigen and antibody bound together) and by foreign sugars on bacterial cell walls. Complement:
•
binds to, and damages, bacterial cell walls, destroying the microbe
•
binds to bacterial cell walls, stimulating phagocytosis by neutrophils and macrophages
•
attracts phagocytic cells such as neutrophils into an area of infection, i.e. stimulates chemotaxis.
The inflammatory response
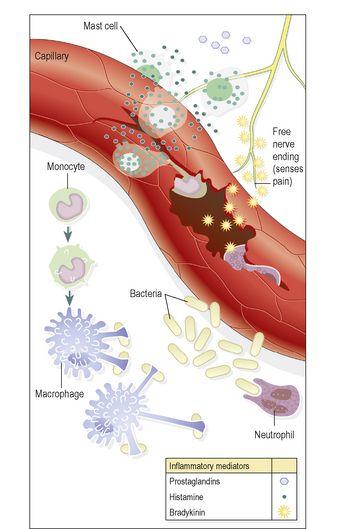
This is the physiological response to tissue damage and is accompanied by a characteristic series of local changes (
Fig. 15.2
). It most commonly takes place when microbes have overcome other non-specific defence mechanisms. Its purpose is protective: to isolate, inactivate and remove both the causative agent and damaged tissue so that healing can take place. The cardinal signs of inflammation are redness, heat, swelling and pain.
Figure 15.2
The inflammatory response.
Inflammatory conditions are recognised by their Latin suffix ‘-itis’; for example, appendicitis is inflammation of the appendix and laryngitis is inflammation of the larynx.
Causes of inflammation
The numerous causes of inflammation may be classified as follows:
•
pathogens (micro-organisms that cause disease), e.g. bacteria, viruses, protozoa, fungi
•
physical agents, e.g. heat, cold, mechanical injury, ultraviolet and ionising radiation
•
chemical agents
–
organic, e.g. microbial toxins and organic poisons, such as weedkillers
–
inorganic, e.g. strong acids, alkalis.
Acute inflammation
Acute inflammation is typically of short duration, e.g. days to a few weeks, and may range from mild to very severe, depending on the extent of the tissue damage.
Most aspects of the inflammatory response are hugely beneficial, promoting removal of the harmful agent and setting the scene for healing to follow.
The acute inflammatory response is described here as a collection of overlapping events: increased blood flow, accumulation of tissue fluid, migration of leukocytes, increased core temperature, pain and suppuration.
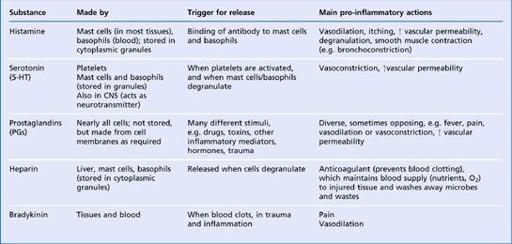
Some of the most important substances released in inflammation are summarised in
Table 15.1
.
Table 15.1
Summary of the principal substances released in inflammation
Increased blood flow
Following injury, both the arterioles supplying the damaged area and the local capillaries dilate, increasing blood flow to the site.
This is caused mainly by the local release of a number of chemical mediators from damaged cells, e.g. histamine and serotonin. Increased blood flow to the area of tissue damage provides more oxygen and nutrients for the increased cellular activity that accompanies inflammation. Increased blood flow causes the increased temperature and reddening of an inflamed area, and contributes to the swelling (oedema) associated with inflammation.
Increased tissue fluid formation
One of the cardinal signs of inflammation is swelling of the tissues involved, which is caused by fluid leaving local blood vessels and entering the interstitial spaces.
This is partly due to increased capillary permeability caused by inflammatory mediators such as histamine, serotonin and prostaglandins, and partly due to elevated pressure inside the vessels because of increased flow. Most of the excess tissue fluid drains away in the lymphatic vessels, and takes damaged tissue, dead and dying cells, and toxins with it.
Plasma proteins, normally retained within the bloodstream, also escape into the tissues through the leaky capillary walls; this increases the osmotic pressure of the tissue fluid and draws more fluid out of the blood. These proteins include antibodies, which combat infection, and
fibrinogen
, a clotting protein. Fibrinogen in the tissues is converted by
thromboplastin
to fibrin, which forms an insoluble mesh within the interstitial space, walling off the inflamed area and helping to limit the spread of any infection. Some pathogens, e.g.
Streptococcus pyogenes
, which causes throat and skin infections, release toxins that break down this fibrin network and promote spread of infection into adjacent, healthy tissue.
Sometimes tissue oedema can be harmful. For instance, swelling around respiratory passages can obstruct breathing, and significant swelling often causes pain. On the other hand, the swelling around a joint cushions it and limits movement, which encourages healing.
Migration of leukocytes
Loss of fluid from the blood thickens it, slowing flow and allowing the normally fast-flowing white blood cells to make contact with, and adhere to, the vessel wall. In the acute stages, the most important leukocyte is the neutrophil, which adheres to the blood vessel lining, squeezes between the endothelial cells and enters the tissues (see
Fig. 4.10, p. 62
), where its main function is in phagocytosis of antigens. Phagocyte activity is promoted by the raised temperatures (local and systemic) associated with inflammation.
After about 24 hours, macrophages become the predominant cell type at the inflamed site, and they persist in the tissues if the situation is not resolved, leading to chronic inflammation. Macrophages are larger and longer lived than neutrophils. They phagocytose dead/dying tissue, microbes and other antigenic material, and dead/dying neutrophils. Some microbes resist digestion and provide a possible source of future infection, e.g.
Mycobacterium tuberculosis
.
Chemotaxis
This is the chemical attraction of leukocytes, including neutrophils and macrophages, to an area of inflammation.
It may be that chemoattractants act to retain passing leukocytes in the inflamed area, rather than actively attracting them from distant areas of the body. Known chemoattractants include microbial toxins, chemicals released from leukocytes, prostaglandins from damaged cells and complement proteins.
Increased temperature
The inflammatory response may be accompanied by a rise in body temperature (pyrexia), especially if there is significant infection. Body temperature rises when an endogenous pyrogen (interleukin 1) is released from macrophages and granulocytes in response to microbial toxins or immune complexes. Interleukin 1 is a chemical mediator that resets the temperature thermostat in the hypothalamus at a higher level, causing pyrexia and other symptoms that may also accompany inflammation, e.g. fatigue and loss of appetite. Pyrexia increases the metabolic rate of cells in the inflamed area and, consequently, there is an increased need for oxygen and nutrients. The increased temperature of inflamed tissues has the twin benefits of inhibiting the growth and division of microbes, whilst promoting the activity of phagocytes.
Pain
This occurs when local swelling compresses sensory nerve endings. It is exacerbated by chemical mediators of the inflammatory process, e.g. bradykinin, prostaglandins that potentiate the sensitivity of the sensory nerve endings to painful stimuli. Although pain is an unpleasant experience, it may indirectly promote healing, because it encourages protection of the damaged site.
Suppuration (pus formation)
Pus consists of dead phagocytes, dead cells, fibrin, inflammatory exudate and living and dead microbes. A localised collection of pus in the tissues is called an
abscess
. The most common pyogenic (pus-forming) bacteria are
Staphylococcus aureus
and
Streptococcus pyogenes.
Outcomes of acute inflammation
Resolution
This occurs when the cause has been successfully overcome. Damaged cells and residual fibrin are removed, being replaced with new healthy tissue, and repair is complete, with or without scar formation.
Development of chronic inflammation
Acute inflammation may become chronic if resolution is not complete, e.g. if live microbes remain at the site, as in some deep-seated abscesses, wound infections and bone infections.
Chronic inflammation
The processes involved are very similar to those of acute inflammation but, because the process is of longer duration, considerably more tissue is likely to be destroyed. The inflammatory cells are mainly lymphocytes instead of neutrophils, and fibroblasts are activated, leading to the laying down of collagen, and
fibrosis
. If the body defences are unable to clear the infection, they may try to wall it off instead, forming nodules called
granulomas
, within which are collections of defensive cells. Tuberculosis is an example of an infection that frequently becomes chronic, leading to granuloma formation. The causative bacterium,
Mycobacterium tuberculosis
, is resistant to body defences and so pockets of organisms are sealed up in granulomas within the lungs.
Chronic inflammation may either be a complication of acute inflammation (see above) or follow chronic exposure to an irritant. Fibrosis (scar formation) is discussed in
Chapter 14
.
Immunological surveillance
A population of lymphocytes, called natural killer (NK) cells, constantly patrol the body searching for abnormal cells. Cells that have been infected with a virus, or mutated cells that might become malignant, frequently display unusual markers on their cell membranes, which are recognised by NK cells. Having detected an abnormal cell, the NK cell immediately kills it. Although NK cells are lymphocytes, they are much less selective about their targets than the other two types discussed in this chapter (T- and B-cells).
Immunity
Learning outcomes