The Washington Manual Internship Survival Guide (24 page)
Read The Washington Manual Internship Survival Guide Online
Authors: Thomas M. de Fer,Eric Knoche,Gina Larossa,Heather Sateia
Tags: #Medical, #Internal Medicine

• Watch for rhabdomyolysis and hyperthermia as complications of prolonged convulsions.
Meningitis
•
Level of urgency: emergent
.
•
Pertinent information: Bacterial meningitis usually presents rapidly with progressive encephalopathy, headaches, and fever and is a neurologic emergency. Viral meningitis/encephalitis generally follows a more benign clinical course; however, it can also leave patients with severe neurologic deficits if not recognized and treated early. In HIV and other immunocompromised patients, fungal infections, such as
Cryptococcus
, should also be considered.
•
History: Patients with bacterial meningitis frequently note generalized myalgias, sore throat, and/or fatigue prior to the major clinical deterioration that brings them to medical attention. Fever, headache, and alteration in level of consciousness are common presenting features. Seizures or photophobia may also be present. An acute confusional state in a febrile patient should always raise the suspicion for bacterial meningitis. Viral meningitis usually presents with symptoms of altered consciousness, fever, personality changes, headache, and flu-like symptoms. Remember to ask the patient about any recent travel or sick contacts.
•
Physical exam: Evaluation of mental status is essential. Meningeal signs should be checked: Brudzinski’s sign (neck flexion resulting in spontaneous flexion of the knees) and Kernig’s sign (passive extension of the knees with hips flexed resulting in eye opening and verbal response). Papilledema suggests increased intracranial pressure, which may result from brain edema or sagittal sinus thrombosis. Rash may suggest a specific infectious etiology, typically
Neisseria meningitidis
.
•
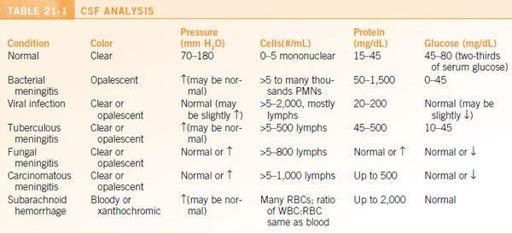
Workup: Neuroimaging should be obtained to rule out a mass as the cause of the altered mental status. Start with a noncontrast head CT. Blood cultures and
urgent lumbar puncture
are required. See
Table 21-1
for CSF interpretation.
•
Treatment: Antibiotics should not be withheld if the head CT and lumbar puncture cannot be obtained rapidly. Obtain blood cultures prior to starting antibiotics, as a significant percentage of bacterial meningitis patients will have bacteremia. Antibiotic coverage should include
ceftriaxone
2 g IV q12h and
vancomycin
dosed for weight and creatinine clearance (see
Chapter 20
). Ampicillin 2 g IV q4h can be considered for patients at risk for
Listeria
. If viral meningitis is suspected, start
acyclovir
10 mg/kg (ideal body weight) q8h empirically while the HSV PCR is pending. The PCR will remain positive for several days after initiating treatment, so acyclovir should not be delayed. See
Table 21-2
for additional treatment recommendations.
OBSTETRICS AND GYNECOLOGY
The OB/GYN History and Physical Examination
•
Perform a basic GYN H&P prior to calling a consult!
•
Gynecologic history:
• Menstrual history:
▪ Last menstrual period (LMP)?
▪ Age at menarche?
▪ Age at menopause? Any postmenopausal bleeding?
▪ If a menstrual problem seems central to the chief complaint, consider asking about menstrual length, inter-menstrual duration, amount of menstrual bleeding (number of pads/day, degree of soilage of pads), and presence of dysmenorrhea.
• Pap history: Date of last pap? Any history of abnormal paps?
• Contraceptive history: Currently using anything to prevent pregnancy?
• Hormone use: Any history of exogenous hormone use (e.g., in postmenopausal women)?
• Sexual history: Currently sexually active? History of any STIs?
• Gynecologic procedure history: Date and type of any gynecologic procedures/surgeries, for example, bilateral tubal ligation (BTL), diagnostic laparoscopy for endometriosis, unilateral or bilateral salpingo-oophorectomy (USO/BSO), loop electrosurgical excision procedure (LEEP)?

•
Obstetric history:
• Ever been pregnant? How many times? Any complications? Any miscarriages?
• If the patient is currently pregnant, ask:
▪ Name of prenatal care provider/clinic? EDC (estimated date of confinement, or due date)?
▪ Any complications during this pregnancy?
▪ If a pregnant patient is admitted to medical services, please give the OB/GYN consultation service a courtesy call.
▪ Any symptoms of vaginal bleeding, leakage of fluid, or decreased fetal movement? Or abdominal trauma? If yes, call OB urgently.
•
Physical exam: The physical exam may help you delineate between gynecologic versus nongynecologic causes of pelvic symptoms. Components may include the abdominal, vaginal speculum, and bimanual pelvic exam; and/or rectovaginal exam; and/or wet prep. What you are able to include will depend upon your level of experience and comfort and access to materials.
• Abdominal exam: Gaseous distension may indicate distended bowels or pneumoperitoneum. A fluid wave may indicate ascites or hemoperitoneum. Solid masses may indicate a benign process, such as uterine leiomyomas, or a malignant process (ovarian or other cancer). Uterine fundal tenderness may indicate pelvic inflammatory disease or postpartum endomyometritis. Adnexal tenderness may be associated with ectopic pregnancy, other adnexal mass/cyst, or ovarian torsion. Suprapubic tenderness may be indicative of cystitis. Call the consult team immediately if either rebound or guarding is present, as this could constitute a surgical emergency!
• Speculum exam: Note any friability, bleeding, or discharge. If you suspect yeast, bacterial vaginosis, trichomoniasis, or PID, swab the posterior fornix (where the discharge pools) and perform a wet prep/KOH prep if possible. If you suspect gonococcal or chlamydial infection, send a urine or endocervical swab test for GC/Ch. Notify the OB/GYN consult team immediately if you see heavy, active bleeding!
• Bimanual exam: Cervical motion tenderness. Note any fundal tenderness or uterine masses. Note any adnexal masses or tenderness. The ovaries are often pea-size or not felt at all. If you suspect pain from a posterior mass, you can perform a rectovaginal exam, in which you can feel masses on the posterior surface of the uterus with the rectal finger.
• Examining the discharge: The GC/Ch test will take about 2 days. However, information can be gathered from pointof-care examination of any vaginal discharge you collected. On the wet prep, you might see white blood cells (associated with PID and tubo-ovarian abscesses), clue cells (associated with bacterial vaginosis), red blood cells (may be present with inflammation or active bleeding), or motile trichomonads. On the KOH prep, look for pseudohyphae (associated with candidiasis) or a positive whiff test (the presence of a fishy odor associated with bacterial vaginosis). A pH test can also be helpful—pH <4.5 may indicate normal vaginal flora or yeast, whereas a pH >4.5 is associated with bacterial vaginosis, trichomoniasis, GC, blood, or menopause.
•
Imaging: Review any abdominopelvic MRI, CT, and ultrasounds that the patient already has. Bear in mind that a CT scan cannot always distinguish the characteristics of adnexal masses well; an ultrasound is better. If further delineation of the pelvic organs is indicated, the OB/GYN consult team should be able to help guide you with which study to order and how it should be performed (sometimes OB/GYN will perform a pelvic ultrasound; at other institutions, it is performed by radiology).
Vaginal Discharge
Vaginitis
•
The most common entities are bacterial vaginosis, vaginal candidiasis, and trichomoniasis.
•
Diagnosis: The key symptoms, signs, and wet prep/KOH prep findings for the most common causes of infectious vaginitis are summarized in
Table 21-3
.
•
Treatment: Listed here are the most common treatments for vaginitis. For additional treatment options, see
www.cdc.gov
.
• Vaginal candidiasis (most commonly caused by
Candida albicans
):
▪
Fluconazole
150 mg PO in a single dose.
▪
Clotrimazole
1% cream 5 g intravaginally for 7 to 14 days (use if pregnant).
• Bacterial vaginosis:
▪
Metronidazole
500 mg PO bid for 7 days.
▪ Metronidazole gel, 0.75%, 5 g intravaginally, once daily for 5 days.

• Trichomoniasis (because this is an STI, encourage the patient to have her partner treated):
▪
Metronidazole
2 g PO in a single dose (preferred).
▪ Metronidazole 500 mg PO bid for 7 days (alternative).
Cervicitis
•
Pertinent information: Most commonly caused by
Neisseria gonorrhoeae
,
Chlamydia trachomatis
.
Trichomonas vaginalis
is also associated with cervicitis.
•
Diagnosis: Suspect if yellow or green cervical discharge. The cervix may be inflamed (e.g., the “strawberry cervix” of
T. vaginalis
). Perform a urine or endocervical GC/Ch probe for definitive diagnosis.
•
Treatment: Adapted from the most recent CDC guidelines at
www.cdc.gov
. If either
gonorrhoeae
or
Chlamydia
is diagnosed, empirically treat for the other. Encourage the patient to have her partner treated.
•
N. gonorrhoeae
:
▪
Ceftriaxone
125 mg IM in a single dose (preferred).
▪ Cefixime 400 mg PO in a single dose (second line, use if above unavailable).
▪
Fluoroquinolones are no longer recommended due to high resistance rates.
•
C. trachomatis
:
▪
Azithromycin
1 g PO in a single dose (for easy dosing or if pregnant).
▪ Doxycycline 100 mg PO bid for 7 days.
Pelvic Inflammatory Disease
•
The presence of cervical motion tenderness, fever, leukocytosis, or worsening pelvic pain should raise suspicion for pelvic inflammatory disease (which can be caused by any one of a number of organisms).
