The Washington Manual Internship Survival Guide (20 page)
Read The Washington Manual Internship Survival Guide Online
Authors: Thomas M. de Fer,Eric Knoche,Gina Larossa,Heather Sateia
Tags: #Medical, #Internal Medicine

Contrast Nephropathy
•
Contrast nephropathy is a common complication of any procedure involving iodinated IV contrast (e.g., radiological studies, angiograms).
•
Risk factors include the presence of renal insufficiency, diabetes, reduced intravascular volume, and large amounts of infused contrast.
•
Strategies for prevention include:
• IV hydration: 1 mg/kg/h of 0.45 or 0.9 NS for 6 to 12 hours before and 6 to 12 hours after the procedure. A sodium bicarbonate solution, 3 ampules of NaHCO
3
(150 mEq total) in 1 L D5W, can also be used. This much NaHCO
3
should not be put in saline due to the high sodium load.
•
N
-acetylcysteine 600 mg bid × 2 doses before the procedure and 2 doses after the procedure may also be added but is of uncertain benefit in most patients.
• Contrast should be given cautiously or not at all to anyone with a Cr > 2.0 and those with acute renal failure.
Gastrointestinal Radiology
•
GI studies can be uncomfortable and require patient cooperation and mobility. If your patient is paralyzed, demented, angry, or delirious, the study will likely be suboptimal or may not be able to be performed.
•
General rules for the “barium versus Hypaque” dilemma (call the radiologist if you have specific questions):
• Barium is bad in pleural or peritoneal spaces so avoid this if perforation, obstruction, or a fistula is suspected. Do not use if the patient is likely to need a laparotomy or CT soon.
• Hypaque is bad in lungs, so avoid in cases of possible aspiration.
Cardiac Studies
In general:
•
No smoking 2 hours prior to test; remove nicotine patches the morning of the test.
•
Small sips of water with medication are fine; however, depending on the type of exam certain cardiac medications (i.e., β-blockers) may need to be held. Consult with the radiology department.
•
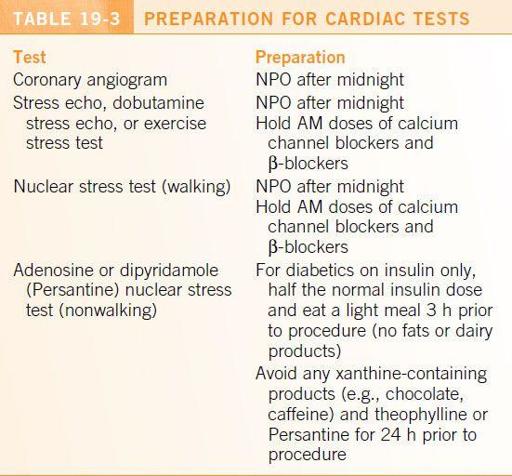
For specific recommendations, refer to
Table 19-3
.
MRI
•
Absolute contraindications are pacemakers, ICDs, cochlear implants, any metal in the globe, and ferromagnetic intracranial aneurysm clips.
•
Relative contraindications are recent operations (less than a few weeks) and recent vascular stenting. Prosthetic hip joints or metal implants are not generally contraindicated, but their artifact may obscure any adjacent lesions. If you have questions, consult MRIsafety.com or call the radiologist.
•
These examinations can be relatively long. The patient must be able to lie still and cooperate—consider mild sedation (e.g., lorazepam) if necessary. The tube is quite small, and patients may get claustrophobic.
Ultrasound
•
Abdominal ultrasounds can be used to evaluate the gallbladder, liver, and kidneys. The pancreas is typically not well visualized so consider CT instead.
•
Ultrasound can also locate pockets of fluid to guide paracentesis or thoracentesis.
•
It is important the patient be made NPO as bowel gas can obstruct the image.
Therapeutic Dosing
20
ANTIBIOTICS
General Principles
Three main issues must be addressed when selecting antibiotics:
•
Expected pathogen and patient demographics (i.e., nosocomial, immunocompromised)
•
Patient allergies and possible drug-drug interactions
•
Renal and hepatic function
Vancomycin
•
Used in severe ß-lactam-resistant gram-positive bacterial infections and to treat gram-positive bacterial infections in ß-lactam allergic patients.
•
Therapeutic trough concentrations (draw 30 min prior to next scheduled dose):
• Uncomplicated skin and soft tissue infections: 10 to 20 μg/mL.
• All other infections: 15 to 20 μg/mL.
•
It can be difficult to initially achieve vancomycin concentrations in this narrow therapeutic range due to significant variability between patients. These therapeutic ranges are narrower than previous recommendations, due to both increased MIC breakpoints for MRSA and increasing reports of vancomycin nephrotoxicity.
•
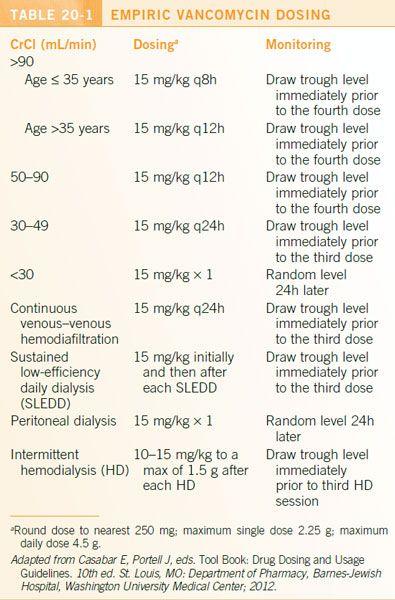
For all patients, the empiric dose of vancomycin should be 15 mg/kg, up to a maximal single dose of 2.25 g and a total daily empirical dose of 4.5 g. Dose should be rounded to the nearest 250 mg.
•
Initial dosing frequency and monitoring are determined by patient factors (
Table 20-1
). Vancomycin should be avoided if possible in those with a CrCl <30 mL/min and not on dialysis.
•
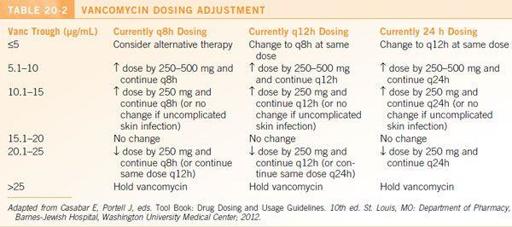
Presuming the current dose is ≤1,500 mg and the patient has stable renal function of ≥30 mL/min, subsequent dosing can be adjusted as shown in
Table 20-2
. Consider obtaining an ID or pharmacy consultation for patients on doses >1,500 mg.
Aminoglycosides
•
Aminoglycosides are primarily used for serious aerobic gram-negative infections; they are also used synergistically with ß-lactam antibiotics in the treatment of select gram-positive infections. Adverse effects include ototoxicity, nephrotoxicity, and neuromuscular paralysis.
•
Serum Cr should be monitored frequently during therapy.
•
Baseline audiometry is recommended for patients whose treatment is planned for >2 weeks.
•
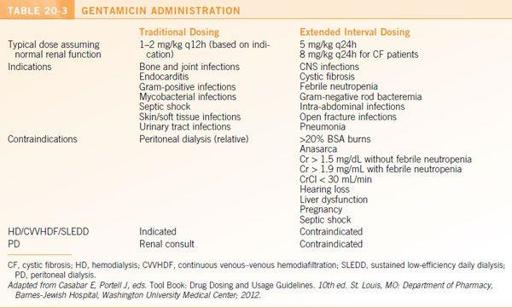
Extended interval (i.e., infrequent) dosing regimens are generally preferred
, but there are contraindications (
Table 20-3
).
•
Calculate the correct
dosing weight
(DW):
• Calculate ideal body weight (IBW):
▪ IBW (male) = 50 kg + 2.3 (height in inches − 60)
▪ IBW (female) = 45.5 kg + 3.4 (height in inches − 60)
•
Underweight
: if IBW > ABW (actual/current body weight) then DW =
ABW
•
Normal weight
: if IBW < ABW < 1.2 (IBW) then DW =
IBW
•
Obese
: if ABW > 1.2 (IBW) then DW =
IBW
+
0.4 (ABW – IBW)
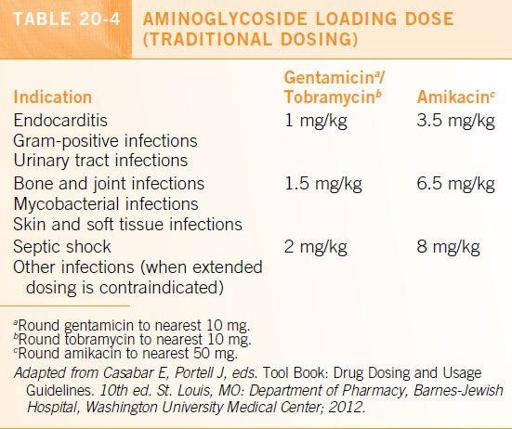
Traditional Aminoglycoside Dosing
•
Calculate a loading dose as per
Table 20-4
.
•
Calculate the maintenance dose as per
Table 20-5
.
•
Initial trough and peak levels are drawn immediately prior to and 1 hour after the start of the third dose. Goal levels when the CrCl is >30 mL/min are presented in
Table 20-6
. Goal level for CrCl <30 mL/min and those on renal replacement therapy are shown in
Table 20-7
.
Extended Interval Dosing
•
Confirm that there are no contraindications to extended interval dosing (EID) (
Table 20-3
).
•
Calculate loading dose based on DW (
Table 20-8
).
•
For non-cystic fibrosis patients, the dosing interval is adjusted using the nomograms in Figure 20-1.
ANTICOAGULATION
•
Before initiating anticoagulant therapy, ensure that the patient has no history of active peptic ulcers, recent stroke or bleeding, or recent surgery.
•
All patients should have a digital rectal examination to document stool occult blood status.
Unfractionated Heparin Weight-Based Dosing
•
Typical initial bolus (round to the nearest 100 units):
• Acute MI: 60 units/kg, maximum 4,000 units
• Acute DVT/PE: 80 units/kg, maximum 6,000 units
• Non-DVT/PE or acute MI: 60 units/kg, maximum of 6,000 units
• High risk of bleeding: Consider smaller bolus
•
Typical initial IV infusion rate:
• Acute MI: 12 units/kg/h, maximum 1,000 units/h
• Acute DVT/PE: 18 units/kg/h. If BMI >40, consider 14 units/kg/h
• Non-DVT/PE or acute MI: 14 units/kg/h
• High risk of bleeding: Consider 12 units/kg/h
•
Check aPTT 6 hours after initial bolus and 6 hours after each rate change. After two consecutive aPTTs are therapeutic (60 to 94 s), the aPTT should be monitored each morning.
