Read The Washington Manual Internship Survival Guide Online
Authors: Thomas M. de Fer,Eric Knoche,Gina Larossa,Heather Sateia
Tags: #Medical, #Internal Medicine
The Washington Manual Internship Survival Guide (4 page)

The Cochrane Database of Systematic Reviews
•
http://thecochranelibrary.net
•
Reviews, analyzes, and synthesizes the best clinical trials by topics.
•
Multidirectional links MEDLINE, EBM, and EUCLID full-text.
•
Subscription required.
PubMed
•
www.ncbi.nlm.nih.gov/entrez/
•
Maintained by the National Library of Medicine.
•
Allows a user-friendly approach to medical literature with built-in search filters. Free.
ACP Journal Club
•
Evidence-based medicine reviews of journal articles.
•
Subscription required.
Useful Formulae
5
A-a O
2
GRADIENT
A-a gradient = PAo
2
– Pao
2
PAo
2
= ([Fio
2
× 713] – PaCO
2
)/0.8
(all units in mmHg)
•
Estimate for upper limit of normal in room air (in mmHg) by age = (age/4) + 4.
•
Causes of increased A-a gradient: V/Q mismatch, intrapulmonary right-to-left shunt, intracardiac right-to-left shunt, impaired diffusion (room air only).
ANION GAP (SERUM)
AG = [Na
+
] - ([Cl
-
] + [HCO
-
3
])
([Na
+
], [Cl
-
], HCO
3
-
] in mEq/L
)
•
Normal = 8–12 mEq/L.
•
See Acid-Base section in
Chapter 18
for differential diagnosis.
ANION GAP (URINE)
UAG = (U
[Na+]
+ U
[K+]
) – U
[Cl−]
(U
[Na+]
, U
[K+]
, U
[Cl−]
in mEq/L)
•
Normal = slightly positive.
•
UAG is
negative
in diarrhea-induced nongap metabolic acidosis (
enhanced
urinary NH
+
4
excretion).
•
UAG is
positive
in distal RTA-induced nongap metabolic acidosis (
impaired
urinary NH
+
4
excretion).
BODY MASS INDEX
BMI = weight/(height)
2
(
weight in kg, height in m
)
•
<18.5 = underweight
•
18.5–24.9 = normal weight
•
25–29.9 = overweight
•
> 30 = obese
CREATININE CLEARANCE/GLOMERULAR FILTRATION RATE
Estimated (Cockcroft-Gault Formula)
CrCl = [(140 – age) × weight]/[serum Cr × 72]
Multiply by 0.85 for women
(weight in kg, Cr in mg/dL)
Estimated (MDRD)
eGFR = 186.3 × (serum Cr)
–1.54
× age
–0.203
× 0.742 (
if female
)
× 1.21 (
if black
)
(eGFR in mL/min per 1.73 m
2
,
Cr in mg/dL)
Measured (24 Hour)
CrCl = (U
[Cr]
× U
volume
)/(P
[Cr]
× 24 × 60)
(Cr in mg/dL, volume in mL, and time in min)
CORRECTED SERUM CALCIUM
Corrected serum Ca = measured [Ca
+2
] + [0.8 × (4.0 – measured albumin)]
([Ca
+2
] in mg/dL, albumin in g/d)
CORRECTED SERUM SODIUM
Corrected serum Na = measured [Na
+
] + [0.016 × (measured [glucose] - 100)]
([Na
+
] in mEq/L, [glucose] in mg/dL)
FRACTIONAL EXCRETION OF SODIUM
FE
Na
= (U
[Na+]
× P
[Cr]
)/(P
[Na+]
× U
[Cr]
) × 100
(U
[Na+]
and P
[Na+]
in mEq/L, U
[Cr]
and P
[Cr]
in mg/dL)
•
FE
Na
< 1% in prerenal states, early ATN, contrast or heme pigment nephropathy, and acute glomerulonephritis.
•
Not valid when diuretics have been given.
FRACTIONAL EXCRETION OF UREA
FE
urea
= [(U
[urea]
× P
[Cr]
)/(P
[urea]
× U
[Cr]
)] × 100
(all units in mg/dL)
•
FE
urea
< 35% in prerenal states.
•
Not affected by diuretics.
MEAN ARTERIAL PRESSURE
MAP = [SBP + (2 × DBP)]/3
OSMOLALITY (SERUM, ESTIMATED)
Calculated serum osm = (2 × [Na+]) + ([glucose]/18) + ([BUN]/2.8)
([Na
+
] in mEq/L, [glucose] and [BUN] in mg/dL)
OSMOLAL GAP
Osmolal gap = measured S
osm
– calculated S
osm
•
Causes of increased osmolal gap: decreased serum water, hyperproteinemia, hypertriglyceridemia, and presence of unmeasured osmoles (e.g., sorbitol, glycerol, mannitol, ethanol, isopropyl alcohol, acetone, ethyl ether, methanol, and ethylene glycol).
RETICULOCYTE INDEX
Reticulocyte index = [measured reticulocyte count × (measured Hct/45)]/maturation factor
Maturation factor = 1 + (0.5 × [(45 – Hct)/10])
•
Good marrow response = 3.0–6.0
•
Borderline response = 2.0–3.0
•
Inadequate response = <2.0
MEDICAL EPIDEMIOLOGY
•
The letters in the following refer to a standard 2 × 2 table presented in
Table 5-1
.
•
Sensitivity:
The percentage of patients with the target disease/condition who have a positive result [A/(A + C)]. The greater the sensitivity, the more likely the test will detect patients with the disease. High-sensitivity tests are useful clinically to
rule OUT
a disease (SnOUT) (i.e., a negative test result would virtually exclude the possibility of the disease).
•
Specificity:
The percentage of patients without the target disease/condition who have a negative test result [D/(B + D)]. Very specific tests are used to confirm or
rule IN
the presence of disease (SpIN).
•
Positive predictive value
(PPV): The percentage of persons with positive test results who actually have the disease/condition [A/(A + B)].
•
Negative predictive value
(NPV): The percentage of persons with negative test results in which the disease/condition is absent [D/(C + D)].
•
Number needed to treat
(NNT): The number of patients who need to be treated to achieve one additional favorable outcome; calculated as 1/absolute risk reduction (ARR), rounded up to the nearest whole number.
•
Number needed to harm
(NNH): The number of patients who, if they received the experimental treatment, would lead to one additional person being harmed compared with patients who receive the control treatment; calculated as 1/absolute risk increase (ARI).

Patient and Staff Relations
6
WORKING WITH ANCILLARY STAFF
•
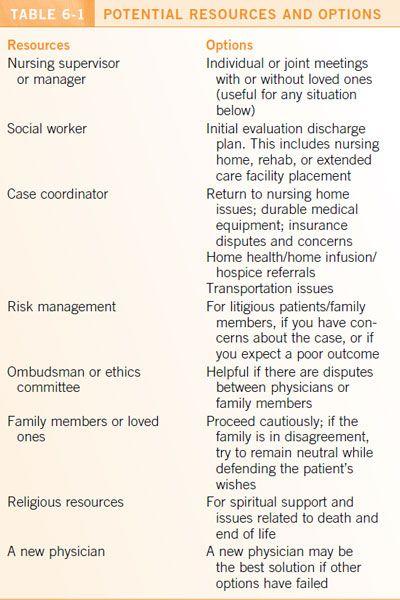
Give specific directions and use your judgment, but also give others a chance to make suggestions and solve problems. Effective use of ancillary staff can greatly increase your efficiency (see
Table 6-1
).
•
A compliment for a job well done goes a long way (others are overworked too), and you will be remembered when you need help. When someone performs exemplary work, let his or her supervisor know.
•
Criticize in private. When done, offer only nonjudgmental and constructive feedback.
•
Regard ancillary staff as fellow members of the patient care team; they are often “bothering” you out of concern for the patient and not to harass you. They have valuable insight that often proves important in patient care.
•
Make efforts to let team members know the plan can save you phone calls and increase sleep.
REFERRING A PATIENT
•
When referring a patient to the ED or another physician, or transferring a patient, always make a courtesy call first.
•
Pertinent information includes the following:
• Who you are.
• Patient identification information.
• Succinct history of the problem.
• Supporting lab data.
• Suggestions for further evaluation.
• Likely disposition of the patient.
• A contact number where you or someone covering for you can be reached for questions or follow-up information.