Read The Washington Manual Internship Survival Guide Online
Authors: Thomas M. de Fer,Eric Knoche,Gina Larossa,Heather Sateia
Tags: #Medical, #Internal Medicine
The Washington Manual Internship Survival Guide (9 page)

•
Chest: Check for chest wall tenderness and any skin lesions. Listen for murmur, rubs, or gallops. Assess JVP.
•
Lungs: Listen for crackles, absent breath sounds on one side, friction rub.
•
Abdomen: Examine for distension, tenderness, and bowel sounds.
•
Extremities: Edema or evidence of deep venous thrombosis. Examine pulses bilaterally in both upper and lower extremities to assess for aortic dissection.
Laboratory Data
•
Obtain an ECG if you haven’t already. Review telemetry, if available.
•
Check ABG if respiratory distress or low saturations are present; serial troponins (q12h × 2), portable CXR.
•
Consider CT angiography or V/Q scan if PE is suspected. Consider contrast CT or TEE if aortic dissection is suspected.
Management
•
Cardiac: If evidence of acute MI on ECG (ST elevation of 1 mm or more in two contiguous leads or new LBBB) and history, call a stat cardiology consult for consideration of reperfusion therapy (thrombolytics or angioplasty). Ensure the patient is on a monitor, has IV access, has oxygen 2 L by NC, and has received an aspirin. Consider administering ß-blockers, nitrates, morphine, heparin (LMWH or UFH). If the chest pain persists, consider loading with clopidogrel, 300 mg PO, and starting a glycoprotein IIb/IIIa inhibitor (e.g., eptifibatide or tirofiban). Metoprolol, 5 mg IV, may be initiated and repeated every 5 minutes for a total dose of 15 mg.
•
Angina: NTG SL, 0.4 mg 3 times every 5 minutes, assuming SBP >90. Consider ß-blockers, IV or transdermal NTG, heparin, and antiplatelet agents. Place on telemetry. If the patient is still having chest pain after NTG SL 3 times, consider administration of morphine and initiating NTG drip to titrate until chest pain free.
•
Aortic dissection: Arrange for immediate transfer to CCU/MICU. Start nitroprusside or labetalol for BP control. Stat vascular/thoracic surgery consultation.
•
Pulmonary: If PE, ensure adequate oxygenation and administer LMWH or UFH.
•
Pneumothorax: Tension pneumothorax requires immediate needle decompression in the second intercostal space in the midclavicular line, followed by chest tube. Other pneumothoraces involving >20% of the lung require a surgery consult for chest tube placement.
•
GI: Antacids such as aluminum hydroxide, 30 mL PO prn q4-6h (avoid in patients with renal failure), famotidine, 20 mg PO bid, or omeprazole, 20 mg PO qday. Elevate the head of the bed, especially after meals.
Refractory Chest Pain
•
Reevaluate the patient for causes of chest pain—has your initial impression changed?
•
Repeat ECG, vital signs, physical exam.
•
For ongoing cardiac ischemia, particularly with elevated troponins and/or ST segment depression, start a NTG drip, consider further antiplatelet agent therapy such as clopidogrel or glycoprotein IIb/IIIa inhibitor, and consider an urgent cardiology consult.
ABDOMINAL PAIN
What are the patient’s vital signs? How severe is the pain? Is this a new problem? If vital signs are stable, inform the nurse you will be there shortly and to call you immediately if things worsen.
Major Causes of Abdominal Pain
Figure 15-1
lists some causes of abdominal pain by location. Generalized abdominal pain may be due to various causes such as appendicitis (at its inception); intestinal infection, inflammation, ischemia, and obstruction; peritonitis of any cause; diabetic ketoacidosis; uremia; sickle cell crisis; acute intermittent porphyria; ruptured aneurysm; and acute adrenocortical insufficiency.
Things You Don’t Want to Miss (Call Your Resident)
•
AAA rupture
•
Bowel rupture, perforation, or ischemia
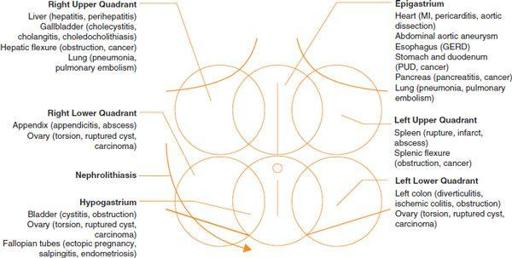
Figure 15-1
. Major causes of abdominal pain.
•
Ascending cholangitis
•
Acute appendicitis
•
Retroperitoneal hematoma
Key History
•
Check BP, pulse, respirations, O
2
saturations, and temperature.
•
Quickly look at the patient and review the chart.
•
Take a focused history, including quality, duration, radiation, changes with respiration, location, N/V (bilious vs. nonbilious), last bowel movement, and any hematemesis, melena, or hematochezia.
•
For women of childbearing age, ask about their last menstrual period.
•
Mesenteric ischemia often has pain out of proportion to examination. Consider this, especially with a history of atrial fibrillation and vascular disease and in elderly patients.
Focused Examination
•
General: Is the patient distressed or ill-appearing?
•
Vitals: Repeat now, especially BP.
•
HEENT: Check for icterus.
•
Chest: Check for any skin lesions. Listen for murmur, rubs, or gallops. Assess JVP.
•
Lungs: Listen for crackles, absent breath sounds on one side, friction rub.
•
Abdomen: Ascultate bowel sounds: high pitched with SBO, absent with ileus. Percussion: tympany, shifting dullness. Palpation: guarding, rebound tenderness, Murphy’s sign, psoas and obturator signs. Assess for CVA tenderness.
•
Rectal: Must be performed. Assess for hemorrhoids and anal fissures. Guaiac for occult blood.
•
Pelvic: If indicated by history.
Laboratory Data
•
Consider CBC, electrolytes, ABG, lactate, LFTs, amylase, lipase, ß-hCG, and UA.
•
Films to consider include flat and upright abdominal films, CXR, and ECG. Abdominal CT, ultrasound, or both may be required.
Management
•
The initial goal is to determine if the patient has an acute abdomen and needs surgical evaluation and treatment.
•
An acute abdomen includes such signs as rebound tenderness or guarding and conditions such as ruptured viscus, abscess, or hemorrhage. See Acute Abdomen section in the General Surgery consult section (Chapter 21).
•
Other conditions can be managed using a more detailed approach, after the acute abdomen has been ruled out.
•
Keep the patient NPO. Ensure large-bore IV access and run maintenance fluids.
ACUTE ALTERED MENTAL STATUS
•
What are the patient’s vital signs? Are the changes acute or subacute? Is the patient confused or is there a change in the level of consciousness? Any recent fall or trauma? Is the patient a diabetic? Does the patient have a cardiac history? Could this be an effect of a prescribed medicine? Could there be an infection? Could this be withdrawal from alcohol or another substance?
•
Initial verbal orders to consider: Think of
TONG
(
T
hiamine,
O
xygen,
N
aloxone, and
G
lucose). Have the nurse obtain blood sugar and oxygen saturations.
•
Acute mental status changes associated with fever or decreased consciousness require that you see the patient immediately.
Major Causes of Acute Altered Mental Status
Think
DELIRIUMS
:
•
D
= Drug effect or withdrawal (e.g., EtOH; narcs, benzos, anticholinergics; especially in the elderly, even in low doses)
•
E
= Emotional (e.g., anxiety, pain)
•
L
= Low Po
2
(e.g., MI, PE, anemia) or high Pco
2
(e.g., COPD)
•
I
= Infection
•
R
= Retention of urine or feces
•
I
= Ictal states
•
U
= Undernutrition/underhydration
•
M
= Metabolic (electrolytes, glucose, thyroid, liver, kidney)
•
S
= Subdural, acute CNS processes (e.g., head trauma, hematoma, hydrocephalus, CVA/TIA)
Things You Don’t Want to Miss (Call Your Resident)
•
Sepsis or meningitis
•
Intracranial mass or increased intracranial pressure
•
Alcohol withdrawal with or without delirium tremens
•
Acute CVA
•
Neuroleptic malignant syndrome
Key History
•
Check BP, pulse, respirations, O
2
saturations, temperature, and blood sugar.
•
Quickly look at the patient and review the chart.
•
Confirm no falls or trauma.
•
Review orders for new meds or narcotics.
•
If possible, take a focused history, including onset and level of responsiveness. Confirm this history with the family or staff.
Focused Examination
•
General: Does the patient appear ill or distressed? Is the patient protecting his/her airway?
•
HEENT: Look for signs of trauma; pupil size, symmetry, and response to light; papilledema and nuchal rigidity.
•
Chest: Check for any skin lesions. Listen for murmur, rubs, or gallops.
•
Lungs: Listen for crackles and equal breath sounds.
•
Abdomen: Look for ascites, jaundice, and other signs of liver disease.
•
Neurologic: Evaluate for weakness, asterixis, rigidity, or asymmetry. Perform a mental status examination.
Laboratory Data
•
Consider CBC, electrolytes, LFTs, ABG, TSH, ammonia level, UA, cultures, ECG, and CXR. Other studies that may be required are lumbar puncture, CT, and EEG.
•
The performance of a head CT before lumbar puncture is controversial but is generally not required for nonelderly, immunocompetent patients who present without focal neurologic abnormalities, seizures, or diminished level of consciousness.
Management
•
Management is based on findings on examination and laboratory data. If meningitis is suspected, lumbar puncture should be performed as detailed above. In addition, empiric antibiotics should be started stat (see Chapter 21, Neurology consult section, for antibiotic choices).
•
Alcohol withdrawal needs to be treated urgently with benzodiazepines, usually with chlordiazepoxide 50 to 100 mg PO q6-8h or lorazepam 0.5 to 1 mg PO/IV/IM q6-8h (prn or scheduled). Thiamine, 100 mg IV/IM, should also be administered, especially before any glucose.
ACUTE RENAL FAILURE
•
What are the patient’s vital signs? How much urine has been produced in the last 24 hours? In the last 8 hours? Does the patient have a Foley catheter inserted? What are the patient’s recent electrolytes, especially potassium, BUN, creatinine, and bicarbonate?
•
If the patient does have a Foley catheter inserted, ask the nurse to flush the catheter with 30 mL NS. If the patient does not have a Foley catheter, ask the nurse to place one now. Tell the nurse you will see the patient shortly.
Major Causes of Oliguria
Oliguria is generally defined as <500 mL of urine per 24 hours. Major causes of oliguria can be broken down as follows:
•
Prerenal
: volume depletion, congestive heart failure, vascular occlusion
•
Renal
: glomerular, tubular/interstitial (acute tubular necrosis caused by drugs or toxins), and vascular
•
Postrenal
: obstruction (BPH), clogged Foley catheter, stones
Things You Don’t Want to Miss (Call Your Resident)
•
Hyperkalemia
•
Severe acidosis
•
Acute, marked uremia
•
Life-threatening volume overload
Key History

