Women's Bodies, Women's Wisdom (42 page)
Read Women's Bodies, Women's Wisdom Online
Authors: Christiane Northrup
Tags: #Health; Fitness & Dieting, #Women's Health, #General, #Personal Health, #Professional & Technical, #Medical eBooks, #Specialties, #Obstetrics & Gynecology

Three months after Doris’s dream experience, I examined her and found that many of her fibroids were gone and so was all of her uterine tenderness. The remaining fibroids seemed to have solidified into a smooth mass that was definitely smaller than it had been at the time of her earlier examination. Doris found that when she takes care of herself and follows her diet, gets exercise, and does some things just for herself, she feels fine and has no pelvic symptoms of any kind. Though her fibroids didn’t disappear entirely, they didn’t grow for years. The last time I saw her she had no tenderness on examination, a testimony to the fact that her endometriosis became very inactive.
Doris used the wisdom of her body to heal some very painful expe riences about which she had not allowed herself to grieve. She was willing to risk completely changing the way she saw herself in the world, a change that often needs to be made if women are to heal at the deepest level. This often involves examining with microscopic honesty how we really feel about being female while also affirming our worth and our inherent goodness. It also may involve cutting way back on our worldly activities and creating a healthful balance between our inner and outer selves.
Uterine prolapse refers to a condition in which the fibromuscular tissue, fascia, and ligaments that normally hold the uterus in place become damaged or relaxed, thus allowing the organ to drop from its normal position in the pelvis. In severe cases, the uterine cervix and the uterus itself may actually protrude from the vaginal opening.
You could liken the pelvic floor supports for the uterus, vagina, and rectum to a floor in a building. In order to support the weight of whatever is on it, the floor must be firmly attached to the structural beams and supports that suspend it. The same is true of the pelvic floor. It relaxes or sags when pelvic muscles have become weak, when there is a genetic weakness in the collagen of the connective tissue, or when it’s damaged from delivering a large baby or from having multiple babies (although if laboring women are properly supported and not encouraged to push too hard, most do not have this problem after delivery). This can show up as prolapse of the uterus (sometimes known as procidentia), prolapse of the bladder (cystocele), prolapse of the rectum (rectocele), or prolapse of all three. If a loop of bowel prolapses into a rectocele, it is known as an enterocele. Sometimes the vagina itself will prolapse following a hysterectomy, resulting in a vaginal vault prolapse.
In moderate cases of prolapse, women experience pressure in the lower pelvis and vaginal area. Sometimes they will feel the cervix moving down their vagina. Others may experience difficulty emptying their bowels completely because of the enterocele.
Prolapses of all kinds are more common in women of northern European heritage and in those with red hair. The reason for this is that blondes and redheads have a collagen layer that is thinner than those who have darker skin. (This is also why those of northern European heritage are more apt to have osteoporosis.) African Americans and those with darker skin are the least likely to experience prolapse.
Treatment
Although approximately 15 percent of the hysterectomies done in the United States are for pelvic organ prolapse, many nonsurgical approaches exist. Mild to moderate pelvic floor sagging can be treated effectively by strengthening the pelvic floor through Kegel exercises (see
chapter 8
). Saida Désilets, Ph.D., author of
Emergence of the Sensual Woman
(Jade Goddess Publishing, 2006), reports that the jade egg exercises have often helped women with mild to moderate prolapse (see
chapter 8
).
Pessaries are also available to hold the organs in place during the day, and most such products are made by the Milex company. Not all gynecologists are familiar with fitting pessaries, so go to one who is well trained in their use. I fitted them for years, especially a soft pessary known as a cube pessary. A woman can easily learn how to insert this pessary herself. It will provide comfort and repositioning of her pelvic organs while strengthening her pelvic floor. Women with more severe prolapses can use larger pessaries. For very mild prolapse, a diaphragm—or sometimes just a tampon inserted in the vagina—can hold things in place.
Hormone Therapy
Women with thinned vaginal tissue secondary to lack of hormones may experience worsening prolapse. A small amount of vaginal estrogen cream along with doing Kegel exercises will often arrest the prolapse while it’s in the mild stage so that surgery can be avoided. Many health care practitioners tell their patients that the prolapse will definitely get worse over the years. But in women who maintain pelvic floor tone (and use hormone replacement to replenish vaginal tissue thickness), this needn’t be the case.
Surgical Approaches
All pelvic floor prolapses are highly amenable to surgery. And over the years, a number of procedures have been developed that allow a woman to keep her uterus by having it surgically suspended in the pelvis rather than removed. This is commonly done via laparoscopy. Surgeons trained in urogy-necology often do this type of procedure. I recommend that all women who are suffering from uterine prolapse consult with a surgeon who is well versed in prolapse corrections that allow the pelvic organs to remain intact. If you opt for a hysterectomy, make sure your surgeon does the surgery in such a way that avoids future vaginal vault prolapse, if possible.
The Mayo Clinic has a good website about prolapse (
www.mayoclinic.org/pelvic-organ-prolapse
). I also recommend the website for the Atlanta Center for Laparoscopic Urogynecology (
www.miklosandmoore.com/pro_treat2.php
), which offers excellent illustrations, explanations, and information about the various treatments.
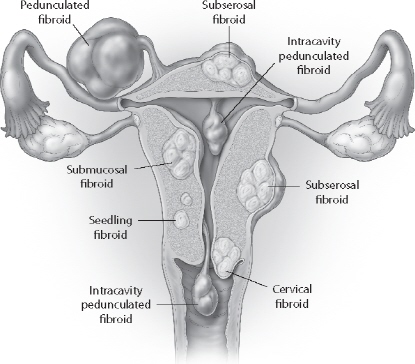
Fibroids are benign tumors of the uterus. They grow in various lo cations on and within the uterine wall itself or in the uterine cavity. (see
figure 11
). Standard medical practice to gauge the size of a fibroid is to compare the size of a uterus with a fibroid with the size of the uterus at various stages of pregnancy. Thus, a woman will be told that she has a fourteen-week-size fibroid if her uterus is as big as it would be if she was fourteen weeks pregnant. Fibroids are made from hard, white gristly tissue that has a whorl-like pattern. They are present in 20 to 50 percent of all women. One of my patients, who watched her fibroid removal via a mirror, later said, “The appearance of the fibroid surprised me. I expected it to be messy-looking. A fibroid looks like a piece of high-density polyethylene plastic, the stuff cutting boards are made of.”
Fibroids are responsible for as many as 33 percent of all gynecolog ical hospital admissions, and they are the number one reason for hys terectomy in this country for women ages forty-five to fifty-four.
23
They are three to nine times more common in black women than in Caucasians. Many women with fibroids are unaware that they have them until they are discovered during a routine pelvic examination. No one knows, from a conventional medical standpoint, what causes them.
Caroline Myss teaches that fibroid tumors represent our creativity that was never birthed, including “fantasy” images of ourselves that have never seen the light of day and creative secrets of our other “selves.” Fibroids also result when we are flowing life energy into dead ends, such as jobs or relationships that we have outgrown. I ask women with fibroids to meditate on their relationships with other people and how they express their creativity. Fibroids are often associated with conflicts about creativity, reproduction, and relationships.
24
I certainly can relate, having developed a large fibroid about five years prior to my divorce. I realized that I had been pouring lots of energy into trying to make a dead-end relationship work. In our rapidly changing culture, where women’s roles are in flux, it is quite obvious to me that conflicts about child rearing, personal expressions of creativity, and changing roles in relationships are a cultural phenomenon, not just an individual one. The fact that so many women have these growths is perhaps evidence of our collective blocked creative energy in this culture.
Symptoms
Most women do not have symptoms from their fibroids. These uterine growths usually come to a woman’s attention on routine pelvic examination. Whether a fibroid is symptomatic has to do with its size and location within the uterus. Those that are located in the muscle wall of the uterus just under the surface (subserosal) may not be symptomatic. But those growing into the uterine lining itself (submucosal) often cause heavy or irregular bleeding. Some fibroids are attached to the inside or even the outside of the uterus by a thin stalk. These are known as pedunculated fibroids. If they are on the outside of the uterus, they are sometimes confused with ovarian tumors. I’ve had two patients who “delivered” pedunculated six-centimeter fibroids through the cervical opening. I simply removed these fibroids by suturing and then severing the stalk. Neither of these women had any further problems.
Women who have both fibroids and endometriosis may experience menstrual cramps, pelvic pain, or both. Most fibroids can be treated conservatively by letting them be and having an examination every six months to a year or so to monitor their growth.
Bleeding
Some women with fibroids have extremely heavy periods, re sulting in anemia, fatigue, and even an inability to leave the house during the heaviest days. If the fibroids are growing quickly, if a woman’s hormones are in flux (which is common around the time of menopause), or if she’s been under a great deal of stress, she can even develop hemorrhaging from uterine fibroids. Some women grow so accustomed to their large monthly blood loss that they don’t even realize how a normal flow would feel. Some may become severely anemic without knowing it.
Fibroid tumors can cause a lot of bleeding because the uterus is endowed with a very rich blood supply. If the fibroid is submucosal, lo cated just under the uterine lining, the body has an especially difficult time with the usual mechanism that stops menstrual flow. Menstrual flow is stopped, in part, by muscular contraction of the uterus, and fibroids may interfere with this mechanism. An endometrial biopsy (taking a sample of tissue from inside the uterus) or sometimes a D&C is necessary in cases of abnormal bleeding to be certain that the bleeding is caused by fibroids and not cancer (though cancer is rarely found). This is especially true for those women who have bleeding at irregular intervals throughout the month.
Fibroid Degeneration
A fibroid may start to degenerate following its rapid growth. This can happen, for instance, during a particularly stressful or emotionally demanding time, during pregnancy, or during the year or so before menopause. Fibroid degeneration can occur when the fibroid outgrows its blood supply. When this happens, the center of the fibroid is deprived of oxygen from the blood, and the nerves deep inside this tissue register a lack of oxygen as pain, in the same way that frostbitten toes do. The pain can be a nuisance, but the condition is not usually dangerous. The degeneration in the center of the fibroid often causes some shrinkage in fibroid size, and on occasion a fibroid shrinks or disappears. The pain usually goes away after a week or so as the nerves adjust.
Pelvic Pressure and Urinary Frequency
Sometimes the position of a fibroid causes symptoms because the fibroid pushes into another or gan, such as the rectum or the bladder. Pressure or a sense of fullness in the rectum, lower back, or abdomen may result. If the fibroid is in the front of the uterus and relatively low, the pressure on the bladder can decrease the bladder’s ability to hold urine, resulting in urinary frequency (having to void in frequent small amounts). These symptoms are annoying but not harmful to the body in general. I’ve never seen an organ contiguous to a benign fibroid that was harmed by the fibroid. An occasional very large fibroid can partially block the ureter (the tube going from the kidney to the bladder) when a woman is lying down. Neither urologists nor gynecologists know for certain whether this situation can eventually cause kidney problems. I have never seen this happen or even heard of it in actual practice! Most women with fibroids large enough to cause urethral pressure prefer surgery simply because they don’t like looking pregnant. Several of my patients, however, have done very well without surgery, and their kidneys are fine. One of these women, who had a very large fibroid uterus for at least ten years, and whose ureter had occasionally shown some blockage from fibroids, began to experience rapid shrinking of her fibroids as she went through menopause. This is common.
Common Concerns
What If I Have a Fibroid?
When fibroids are felt for the first time, I recommend a pelvic ultrasound to measure them and to check out the sta tus of the ovaries. Sometimes it’s impossible on a pelvic exam to tell the difference between an ovarian growth and a fibroid on the uterus.
