Women's Bodies, Women's Wisdom (40 page)
Read Women's Bodies, Women's Wisdom Online
Authors: Christiane Northrup
Tags: #Health; Fitness & Dieting, #Women's Health, #General, #Personal Health, #Professional & Technical, #Medical eBooks, #Specialties, #Obstetrics & Gynecology

Another issue that affects a woman’s pelvic organs is competition among her various needs. When her innermost needs for companionship, sexual and/or creative expression, and emotional support are in competition with her outer needs for success, autonomy, and approval, this situation may manifest in her inner pelvic organs, the ovaries and the uterus. For centuries, our culture has taught women that we can’t be both emotionally fulfilled and financially successful; we can’t have it all. Women are not usually taught to be com petent in handling economic and financial assets because the patriarchal system depends on women being dependent. (This is rapidly changing. While women made up only one-third of the workforce in 1969, they make up nearly half the workforce today—although they typically earn only 78 cents for every dollar men earn. More than 39 percent of American women are their family’s primary breadwinners, and another 24 percent bring home at least a quarter of the family’s bacon. A mere 20.7 percent of households in the United States today reflect the traditional model of a working father and a stay-at-home mother.)
9
The uterus is related energetically to a woman’s innermost sense of self and her inner world. It is symbolic of her dreams and the selves to which she would like to give birth. Its state of health reflects her inner emotional reality and her belief in herself at the deepest level. The health of the uterus is at risk if a woman doesn’t believe in herself, is excessively self-critical, or is putting too much of her energy into a dead-end job or relationship.
Pelvic pain can occur in one pelvic organ such as an ovary, in several pelvic organs, or throughout the pelvis, even if all the pelvic organs have been removed. A certain percentage of women with chronic pelvic pain are not helped by surgery or medical treatment. Though hysterec tomy can relieve chronic pelvic pain in some, almost one-quarter of those women who undergo hysterectomy for this condition fail to get pain relief.
10
Women who have chronic pelvic pain often have complex psychological and emotional histories. Studies have found that they are more likely to have sought treatment for unrelated somatic complaints, have a higher total number of sexual partners, and are significantly more likely to have experienced previous significant psychosexual trauma.
11
Their physical pain is also related to unfinished emotional pain in either past or current relationships with partners or with jobs, sexual abuse, emotional abuse, or rape (on any level). Emotional stress in a woman’s personal or professional life that she perceives to be unresolvable is a big contributor to pelvic pain. Unresolved traumatic events from the past live in the energy system of the body, even after the pelvic organs have been removed surgically. I commonly see pelvic pain flare-ups in women who uncover incest memories, visit the place in which the incest occurred, or work at jobs that control them but in which they feel they must continue to work. I tell these women that, through their pain, the body is asking them to pay attention to it and take care of it. The body, in its wisdom, wants to bring their attention back to the physical site of their emotional pain so that they can begin the healing process.
In many cases of chronic pelvic pain, no physical cause can be found and therefore the medical profession does not take it seriously. But chronic pelvic pain that comes from unresolved, past emotional pain is real—it is not just “in the head.” Pain is patterned or stored physically and chemically in our nervous, immune, and endocrine systems; it is in the bodymind. It cannot simply be cut out sur gically.
Physical therapists Belinda and Larry Wurn have discovered that women who’ve had infections, trauma, or multiple surgeries often have adhesions that pull on nerves and glue organs together, so pelvic pain with intercourse or with one’s period is common. The Wurn technique has been shown to decrease pain significantly when adhesions are the problem. (See
chapter 5
.)
Endometriosis is a mysterious but increasingly common condition. The tissue that forms the lining of the uterus, the endometrial lining, normally grows inside the uterine cavity (and is responsible for monthly menstrual cycles). In endometriosis, for some reason, this tissue grows in other areas of the pelvis and sometimes even outside the pelvis entirely. (There are documented cases of endometriosis in the lining of the lungs and even in the brain.) The most common site for endometriosis is in the pelvic organs, especially behind the uterus, but it can also occur on the pelvic side walls (which surround the internal organs in the pelvic cavity), and sometimes on the bowel.
Endometriosis is sometimes associated with infertility and pelvic pain, though not always. Since fibroids and endometriosis are often present in the same individuals at the same time, everything I say about fibroids often applies to endometriosis as well. Like fibroids, endometriosis is related to diet, immunity, hormone levels, and blocked pelvic energy.
Endometriosis is an illness of competition.
12
It comes about when a woman’s emotional needs are competing with her functioning in the outside world. When a woman feels that her innermost emotional needs are in direct conflict with what the world is demanding of her, endometriosis is one of the ways in which her body tries to draw her attention to the problem.
Alycia’s case illustrates this point well. When she first came to see me with pelvic pain and endometriosis, she related that she’d become pregnant in college and had had an abortion. Though she had felt torn over this decision, and though at some level she had really wanted to have the baby, she also felt compelled to finish college and go to law school. She told me that she had never been able to resolve the conflict between her desire to have a baby and her competing desire to be creative in the outer world of law and business. It is this conflict that is so often associated with chronic endometriosis and pain. The conflict articulated by Alycia is almost archetypal, and I see it reg ularly. Women are now part of the traditionally male world of competition and business. And many do not get emotional support in their homes or personal lives. Others have abandoned the notion that they even have emotional requirements. A great many of the women I’ve seen who have endometriosis drive themselves relentlessly in the outer world, rarely resting, rarely tuning in to their innermost needs and deepest desires. It makes perfect sense that so many women would have this disease at this time in our history. One Jungian analyst has referred to endometriosis as “a blood sacrifice to the Goddess.” It is our bodies trying not to let us forget our feminine nature, our need for self-nurturance, and our connection with other women.
Historically, endometriosis was called the “career woman’s disease.” Women who delayed childbearing were felt to be at greatest risk for it. In the recent past, many women with endometriosis were told that if they’d stay home and have babies, they would be okay. This is a controversial assertion— besides being an offensive one—since some recent studies show that there is no difference in the incidence of endometriosis in women who have been pregnant and those who have not. David Redwine, M.D., an internationally known endometriosis expert, concludes that pregnancy offers no protection against endometriosis. What would protect against the disease would be business and personal environments that don’t require a mental-emotional split. This split is why so many women are dropping out of the corporate world to work at home or start their own businesses. Regardless of what she chooses, a woman with endometriosis can work toward healing herself immediately, starting with a willingness to listen to her body.
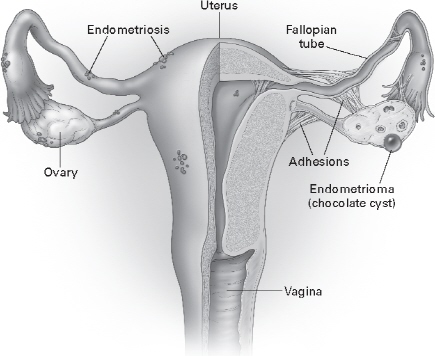
Endometriosis, which can grow virtually anywhere in the body, is usually limited to the pelvis lining, the uterine surface, and the ovaries, where it shows up as endometriomas (also called chocolate cysts).
Symptoms
Endometriosis is classically associated with pelvic pain, abnormal menstrual cycles, and infertility. These symptoms vary a great deal from woman to woman. Some women with advanced endometriosis have never had any symptoms at all and don’t even know that they have the disease until their doctor diagnoses it. Others, with only minimal endometriosis, may nonetheless have debilitating pelvic pain and cramps almost continuously. Most women are somewhere in between these two extremes. The most common area for endometriosis to occur is behind the uterus in the area between the uterus and rectum, known as the cul-de-sac of Douglas. Endometriosis in this area can cause painful intercourse, rectal pressure, and pain with bowel movements, especially before a period.
Diagnosis
Endometriosis of the pelvic cavity can be diagnosed definitively only via laparoscopy, though I often suspect it in women whose symp toms are consistent with endometriosis, such as a history of pelvic pain and intermenstrual spotting. In a few rare cases, it can be seen during a pelvic exam if endometrial lesions are present on the cervix, vagina, or vulva. Unfortunately, studies show that the average woman with endometriosis goes to about five doctors before the diagnosis is made because many other medical conditions, such as irritable bowel syndrome, mimic endometriosis.
Some authorities believe that you can find endometriosis in any one if you look hard enough.
13
I agree with this. I’ve found endometriosis in a surprising number of completely asymptomatic women at the time of laparoscopic tubal ligation. Neither they nor I would have suspected it.
What I’d like to know is the incidence of endometriosis in women who have no problems. I believe that all women probably have embryonic cells in their pelvic cavities that could grow into endometrial tissue. But if all of us have the potential for endometriosis, why do some women develop symptoms while others do not? Until further research clarifies this, the answers lie within the individual woman. It is up to her to decipher what her symptoms are trying to tell her and to take steps to change the factors that favor the growth of endometriosis.
Common Concerns
Why Do So Many Women Have Endometriosis?
When I was in training, we didn’t see nearly as much endometriosis as we’re seeing now. There are a number of reasons for the perceived increase in the disease. First, with the advent of laparoscopy, we are diagnosing it more frequently. The patient is in and out of the hospital on the same day. The ease of looking into the pelvis without doing major surgery results in lap aroscopy being offered rather routinely to patients who have pelvic pain.
Another factor in the apparent increase in incidence of endometriosis is that women today are delaying childbearing. When they do have children, they are having fewer of them—which means they have a greater number of menstrual cycles than women did in the past. Since endometriosis is a hormone-dependent dis order, when the body has relatively high circulating estrogen levels without the break that occurs during pregnancy and nursing, endometriosis becomes more likely.
Is Endometriosis Hereditary?
Endometriosis often runs in families, so there is some hereditary link. I’ve seen patients whose sisters and moth ers all had it. But having a close relative with endometriosis does not guarantee that you’ll have it, too, especially if you live your lives in different ways. The genetic potential for endometriosis does not have to manifest unless your environment and health habits promote it. The standard nutrient-poor American diet, which favors cellular inflammation and hormone imbalance in susceptible individuals, contributes to endometriosis and is often the type eaten by families who have endometriosis. In my clinical experience, intake of conventionally produced dairy foods and a refined-food diet are especially associated with exacerbating the pain of endometriosis.
Will Endometriosis Interfere with My Fertility?
Many endometriosis pa tients are fertile women whose main problem is pain. Endometriosis does not cause infertility, but it is felt to be a major contributing factor. Currently, 40 to 50 percent of women who have a laparoscopy to determine the cause of their problems with infertility are found to have endometriosis.
14
Many women with endometriosis have the massive pelvic scarring usually associated with infertility. Dr. Redwine says, “Studying the disease among predominantly infertile women only serves to confuse the issue.”
15
Whatever is causing the endometriosis symptoms may also be responsible for the infertility, but one doesn’t cause the other.
16
So What Causes Endometriosis?
Medical theories about endometriosis abound, but no one really knows what it is and why so many women seem to have it now. The classic theory is that endometriosis results from retrograde menstruation, or menstruating backward, so that some of the menstrual blood and tissue that line the uterus go back up the fallopian tubes, then implant in the pelvic tissue and begin to grow.
17
Since retrograde menstruation probably occurs in every men struating woman at some point, this doesn’t explain why some women get the disease and others don’t. Another theory is that pelvic tissues spontaneously convert to endometrial tissue, possibly due to irritation or hormonal activity from environmental toxins such as dioxin, which can have estrogen-like activity.
