Women's Bodies, Women's Wisdom (99 page)
Read Women's Bodies, Women's Wisdom Online
Authors: Christiane Northrup
Tags: #Health; Fitness & Dieting, #Women's Health, #General, #Personal Health, #Professional & Technical, #Medical eBooks, #Specialties, #Obstetrics & Gynecology

3. Don’t douche.
Using vaginal douches not only is unnecessary but also been associated with low infant birth weight and bacterial vaginosis.
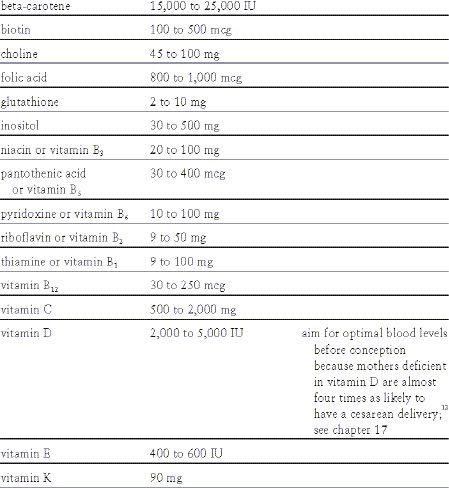
4. Take supplements.
And start before conception, if possible. (One recent study showed, for example, that women who at conception had the lowest levels of vitamin B12—necessary for red blood cell production and a healthy nervous system—had up to five times the risk of having a child with a neural tube defect than women with the highest levels.)
11
For the best results, be sure the potency of the supplements you take is guaranteed and that the supplements are manufactured according to GMP (good manufacturing practices) standards. I recommend a daily supplement with the following vitamins and minerals at the following levels:
V
ITAMINS
12
M
INERALS
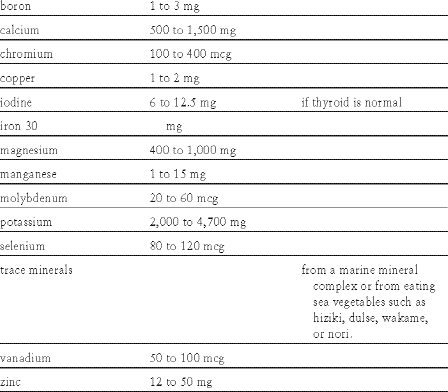
The iodine recommendation may seem high, but a great deal of evidence indicates that the current RDA for iodine in pregnancy is woefully inadequate for optimal fetal health. Given the link between iodine and fetal brain development, I recommend iodine levels beyond the current RDA’s. See the iodine discussion in chapter 10. By the way, not only are adequate vitamins important to the baby, but they can be important to the mother. For example, a 2008 study found that vitamin D deficiency is linked to bacterial vaginosis (a common vaginal infection) in the first trimester of pregnancy. As vitamin D levels improved, according to the researchers, the prevalence of bacterial vaginosis decreased.
13
5. Eat enough omega-3 fats, especially DHA.
Essential fatty acids (also called polyunsaturated long-chain fatty acids or PUFAs) help the body fight and ultimately stop cellular inflammation. Eating enough may help prevent prematurity and low birth weight.
14
The main source of omega-3s are fatty fish, eggs, nuts, seeds, sea vegetables, and green leafy vegetables such as spinach, broccoli, cabbage, collards, and kale. Unprocessed vegetable oils (most notably flaxseed, macadamia nut, and hempseed oils) are also good sources.
6. Get regular exercise.
Regular exercise during pregnancy reduces the odds of giving birth to newborns with excessive birth weight by 23–28 percent, according to a 2009 study from Norway.
15
7. Start a meditation program.
Calm Birth is a form of childbirth preparation that uses proven mind-body and breathing techniques to help create an atmosphere of calmness that decreases fear, pain, and complications for both pregnancy and childbirth. Many medical cen ters now use this program with good results. The three main methods Calm Birth teaches are the Practice of Opening (allowing the parents-to-be to experience remarkable access to the development of their unborn child), Womb Breathing (where women learn to breathe into their energy bodies to reach full potential in childbirth and also to enrich the child), and the Giving and Receiving Meditation (which teaches how to transform the energy of fear, anxiety, and tension into light in your own body, and breathe it out). The preface to the program states, “When pregnant women practice meditation, an empowering sense of safety and wholeness is generated from the inside. The Calm Birth Methods were developed to give women direct ways to raise the quality of health in childbirth whether or not medical interventions are applied. These methods have been shown to lower the impact of interventions and also lower medical costs and risks.” This is a very powerful program, and I highly recommend it. For those who can’t find a Calm Birth practitioner in their area (currently, most are on the West Coast), the orga nization also offers a CD called
Calm Birth,
as well as a postnatal program called
Calm Healing
. (For more information, contact Calm Birth at 541-488-2563 or visit their website at
www.calmbirth.org
.)
8. Get massage.
Massage has wonderful benefits, including boosting endorphins and decreasing stress hormones. Research by Tiffany Field, Ph.D., founder and director of the Touch Research Institute at the University of Miami School of Medicine, has done extensive research showing that pregnant women who receive massage experience reduced anxiety, improved mood, reduced back pain, and increased sleep. They also have fewer complications in labor, less labor pain, and fewer premature babies.
16
(For more information, see the Touch Research Institute’s website at
www.miami.edu/touch-research
.) A twenty-minute foot rub at the end of a day of work is a good alternative if you can’t do a full-body massage.
9. Expose yourself to natural light.
Morning bright light significantly helps reduce depression in pregnant women, according to a 2002 Yale study. Researchers found that after three weeks of morning bright light ther apy, depression ratings improved by 49 percent, and benefits were seen through five weeks of treatment. They also found no evidence of ad verse effects of light therapy on pregnancy. Because drugs for depression are best avoided, if possible, during pregnancy, and because depression in pregnancy may be a risk factor for preeclampsia, this is significant news.
17
Despite a great deal of research in this area, the rate of premature birth hasn’t declined in the past fifty years. It occurs in about 13 percent of pregnancies and contributes to more infant deaths than any other factor except severe birth defects.
18
Assisted reproductive technologies have increased the number of multiple gestations—and thus increased the number of premature babies. The increasing popularity of labor inductions has played a part, too; we are now seeing an increase in late-term prematurity (thirty-seven weeks or so), which puts far too many babies in the intensive care unit because of problems with lung maturity. These induction-related prematurities would be preventable if women were encouraged to go into labor normally.
19
Though many drugs have been used to try to stop labor, these have only limited benefit and haven’t significantly affected the prematurity rate. Until the mind-body-lifestyle connection in premature birth is addressed, the rate is unlikely to change. It is well documented that uterine blood vessels are exquisitely sensitive to the effects of sympathetic nervous system stimulation and that the hormones associated with stress of all types can cause changes in blood flow to the fetus.
20
In a study of sixty-four women, for instance, Lewis Mehl-Madrona, M.D., Ph.D., found that a range of the psychological factors (fear, anxiety, and stress; lack of support from the woman’s partner; poor maternal self-identity; negative beliefs about birth; and lack of support from friends and fam ily) predicted deliveries that required obstetrical intervention ranging from cesarean section to oxytocin augmentation or induction. In an other study, hypnotherapy was found to play a statistically significant role in preventing negative emotional factors from leading to C-section or oxytocin augmentation or induction. Dr. Mehl-Madrona has also used hyp notherapy to help women avoid giving birth prematurely. Each woman who received hypnotherapy was reassured that she was doing the best she could, asked to state what her stresses were, and then given the sug gestion that her body would know what to do to keep her baby safe. As fear and anxiety decreased through supportive hypnotherapy, so did adverse outcomes.
21
One study followed women with a history of three consecutive miscarriages for which no medical cause could be found. On their subsequent pregnancy, they had a suture placed in their cervix to hold the pregnancy in place. Eighty-nine percent of these women went on to have severe postpartum depression, compared with only 11 percent of the control group who experienced mild to moderate depression. The authors of this study concluded that “these women were forced into motherhood.”
22
When severe emotional conflicts about motherhood aren’t dealt with consciously, they can be exacerbated postpartum and result in emotional breakdown. It is clear that adverse pregnancy outcomes could be prevented with approaches that help a woman name and work through the particular stresses that can so profoundly affect her pregnant body and her unborn baby.
One of the most underacknowledged but important factors in poor pregnancy outcome is that the pregnancy is unwanted or unplanned or there is some unrecognized ambivalence around it. Current data suggest that at least 50 percent of all pregnancies are unplanned.
23
It’s much more difficult to ascertain which ones are unwanted because many women adjust well to unplanned pregnancies and end up desiring them. Maternal ambivalence about pregnancy is a setup for complications unless a woman can resolve her feelings during the pregnancy. (See
chapter 11
.) A woman who feels (usually unconsciously) that she must end her pregnancy as soon as possible to get on with her life, get the pregnancy over with, or “get her body back” may go into premature labor or develop another condition that ends her pregnancy sooner. Numerous studies have doc umented the profound effects of psychological variables on birth outcome—in other words, prematurity may correlate with poor maternal emotional and physical investment in the pregnancy.
24
Animal studies have indicated that the death of a baby in utero may also be related to marked maternal anxiety. In pregnant monkeys, guinea pigs, and rab bits subjected to emotional stress, the uterine and placental blood flow were constricted from adrenaline released in response to the stress. As a result, the fetuses did not receive enough oxygen, and many died of asphyxia. Marked maternal anxiety and stress also causes uterine blood vessels to constrict via hormonal and neurotransmitter release into the circulation. This reduces oxygen to the baby and may well be related to pregnancy complications, such as placental abruption, pla centa previa (a condition in which the placenta covers the cervical opening, which can lead to bleeding and/or prematurity), a prolapsed umbilical cord, a cord around the neck, or breech presentation.
25
The good news is that mothers can learn to com municate healthful emotions to their babies regardless of their circumstances. After all, the baby is a part of a pregnant woman’s own body. When women learn how to get in touch with their inner guidance systems, they can learn how to keep their babies safer and even interrupt premature labor and halt the progression of toxemia. It’s really very simple. You just take a deep breath, set an intention to connect with your baby, and tell the child that you are doing everything in your power to keep him or her safe and healthy. Over time, you’ll be able to get a feel for your baby’s response. And remember that your child knew what he or she was getting into when the baby came to you. Of course, women who develop premature labor and toxemia also have to be willing to stop work, rest more, and change any harmful patterns of behav ior and thought. The pioneering work of Dr. Lewis Mehl-Madrona has shown that prenatal intervention consisting of social support, education, and labor support in a group of minority women reduced alcohol intake, smoking, and stress, and also improved birth outcome significantly.
26
T
O
E
NHANCE
I
DEAL
G
ESTATIONAL
A
GE
If you are at risk for premature labor:
