Joy, Guilt, Anger, Love (20 page)
Read Joy, Guilt, Anger, Love Online
Authors: Giovanni Frazzetto
Tags: #Medical, #Neurology, #Psychology, #Emotions, #Science, #Life Sciences, #Neuroscience

Even if, as human beings, we may universally experience grief and share a few of its common biological components, in its detail it varies greatly from individual to individual. Again, some of the variation stems from cultural rituals. I see my grandmother’s bereavement in the flowers she buys and the candles she lights, in the modest dark clothing she wears, in her dusting of the telescope, in the pauses she makes when she speaks about Granddad, and in the fish soup she cooks in his honour for family gatherings, because that is what grief looks like in her: none of which can be conveyed by the mere word ‘grief’ – or prolonged grief disorder, for that matter.
The psychiatrist Ronald Pies has used Wittgenstein’s concept of ‘family resemblances’ to express how difficult it is to describe mental states, especially in the context of psychiatry.
35
Wittgenstein suggested that when we look at a family portrait, most probably there will be no one feature shared by all members of the family. However, if we inspect the picture closely, a few resemblances will become apparent. Five members might all have freckles, and three of those five might also have blue eyes, as do several non-freckled people in the portrait; three other members of the family may be the same height. Taken in combination, such features are indications that the people pictured are all related, even though there is no single feature present in all. The same applies to psychiatric disorders. No two people sharing a diagnosis of depression are exactly the same. And, for sure, where grief is concerned one size does not fit all either. There will always be huge variation between individuals in their experience of grief. Equally, the course of each individual’s path to recovery will be strictly personal. Categories in psychiatry are black or white diagnoses: you either have the disorder or you don’t. But when one is making a detailed study of symptoms, or looking for the neurological or genetic factors underlying a disorder, methods of assessment and measuring systems that account for diversity will be more helpful.
The molecule of sadness
One of the most pervading popular narratives about depression is that it is the outcome of a chemical imbalance – more specifically, a decline in the level of neurotransmitters in the brain.
Neurotransmitters, the molecules that relay messages between neurons in the brain, have entered everyday vocabulary. Here are just a few examples: we find ourselves associating the pleasure gained from sport with the release of endorphins. We speak of an ‘adrenalin high’ when it keeps us alert and insomniac after a test, a performance or an important meeting. Occasionally we mention the hormone cortisol to describe or justify our levels of stress. But if there is one molecule that has truly become a household term, a topic for tube or dinner conversations, a recurrent word in science magazine titles, it must be the neurotransmitter serotonin. I have often heard and cringed at statements like: ‘My serotonin levels must be low today’ or ‘That man needs to boost his serotonin’.
Serotonin has a simple molecular structure (Fig. 11): twenty-five neatly arranged atoms. It is heralded too easily as
the
molecule of happiness, used as a sloppy shorthand term for the status of our brain and for our well-being. Serotonin has become so popular that it is possible to spot its molecular structure printed on mugs, T-shirts, postcards, moulded as jewellery and even tattooed in praise of its properties as a mood-lifter.
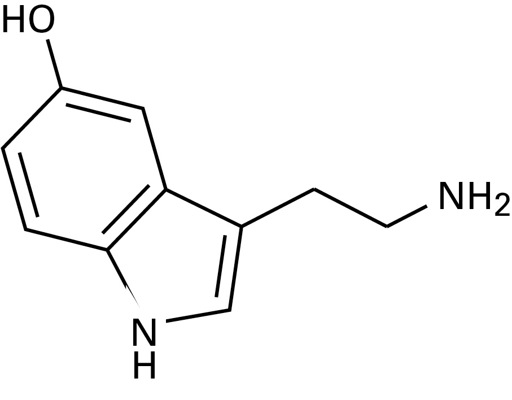
Fig. 11 Molecular structure of serotonin
Serotonin is not exclusively present in the brain. Approximately 90 per cent of the entire amount of serotonin in the body is in fact stored in the intestines. There, it facilitates gut movements through the regulation of the expansion and contraction of blood vessels, and is also involved in the function of platelets, the blood cells that promote the coagulation of blood and the closure of a wound. Only the remaining 10 per cent of serotonin accomplishes its other duty, that of neurotransmitter in the brain, where it is produced by dedicated serotonergic neurons, mostly in a structure called the raphe nuclei. These are located in a central part of the brain, along the midline above the brainstem, and have neuronal connections extending to almost every part of the central nervous system.
The discovery that mood may correspond to a neurochemical imbalance in the brain is to be traced back to the 1950s. It was based on a series of unexpected observations, some of which were made in animals, that a few drugs interfered with mood. Some drugs improved it, some worsened it. Those which improved it raised the levels of neurotransmitters. Those which worsened it pushed the levels of neurotransmitters down. Most of these drugs targeted the system of monoamines, which are a family of molecules in the brain that include norepinephrine and serotonin. For instance, doctors had noticed that the administration of the drug reserpine lowered people’s mood. Later, it was found that reserpine had sedating effects in rabbits, and also corresponded to a lowering of serotonin.
36
The accumulation of data of this kind led to the formulation of a simple hypothesis: depression equated to a decline and elation to an excess of those amines.
37
This theory had a tremendous impact on psychopharmacology. Pharmaceutical companies began to synthesize drugs that worked to increase the presence of neurotransmitters.
In order to understand how drugs really affect serotonin, let’s brush up on some of the basics of neurochemistry.
The hundred billion neuronal cells that make up your brain do nothing but talk to each other. Remarkably, the communication goes on without the neurons having to touch. The ‘language’ in which messages are conveyed consists of sequences of neurotransmitter molecules and the dialogue between cells takes place across a tiny empty space called the synapse, the point of encounter between neurons. Picture this space as a channel separating two shores, and the neurochemical shuttling of information between one neuron and the other as an old-fashioned exchange of letters, with neurotransmitters like serotonin being reliable postmen on boats – my granddad could have been one. Whenever a neuron needs to communicate a message, it launches the relevant neurotransmitter into the channel. Waiting on the opposite shore are receptors, the recipients of the letter. There are at least fifteen different types of receptor that can receive the message from serotonin, each with a different role in coordinating various aspects of mood (in chapter 3, for instance, I mentioned the serotonin receptor 1A that contributes to keeping anxiety at bay via its inhibitory function). The delivery system is extremely accurate and, as it were, confidential: the message can only be read by its intended recipient – that is to say, serotonin binds only to serotonin receptors. The recipients do not keep the message. After having been opened and read, the letters are sent back into the channel, the synaptic cleft. In the meantime, the sending neuron has dispatched more letters across the channel, so at some point there may be too many boats floating around – too much serotonin. When that happens, those extra boats must be cleared because the whole system strives for an equilibrium.
There are two main strategies by which the serotonin is cleared from the channel to keep the right balance. The first is through the action of enzymes that degrade it. Maintaining the marine metaphor, think of such enzymes as if they were sharks that chew up the floating serotonin. One such shark is the infamous MAOA, a major serotonin degrader. When drugs were first developed specifically to maintain high levels of serotonin there was a class that were, in fact, inhibitors of MAOA.
The second strategy is to clear the synaptic cleft of serotonin by sending it back to where it came from, a sort of conscientious paper recycling. This is done through the action of dams or embankments on the neuron of origin that suck up whatever neurotransmitters are present in excess.
38
Serotonin has one such embankment dedicated to its ‘re-uptake’: it is a large protein on the outer walls of the neuron, known as the serotonin transporter. Too soon this became a target for drug treatment in the quest for enhanced levels of serotonin. A new class of medications exploded on to the scene, the selective serotonin re-uptake inhibitors (or SSRIs). Prozac was born, and following its incredible commercial success a host of similar drugs were introduced. Medications like Prozac, Zoloft, Sertraline or Paxil all work by inhibiting the serotonin transporter and trying to increase the amount of serotonin available for its receptors – the recipients on the other shore.
Ever since their introduction into the pharmaceutical market, SSRIs have enjoyed an impressive career, at least from an economic perspective. Over thirty antidepressants have been released. In the United States alone, one of the countries with the highest consumption, in 2011 the number of antidepressant prescriptions went beyond 250 million, over a hundred million more than in 2001.
39
These remarkably high figures correspond to sales equivalent to $25 billion.
Yet this economic success is not matched by improvement in the population’s overall mental health, if we consider the high incidence of depression in the world. In Europe, the largest toll out of the total burden of illness is attributable to psychiatric disorders.
40
That a deficiency in serotonin is the cause for a low mood is not a definitively ascertained hypothesis and results from ongoing work aimed at resolving this question remain contradictory. Apart from some of the general and opening stages in the chain of reactions that I have just described, the exact molecular mechanism by which common antidepressants work is not fully understood. We have a fairly neat picture of how serotonin accomplishes its role in the synapse, but our knowledge of exactly how the mechanism then translates the message into cell events and mood changes and of what makes the drugs effective is far from complete. Regardless of that, for a couple of decades pharmaceutical companies have used a simple and easy-to-remember slogan telling us that when it comes to serotonin, the more of it you have, the better you feel. Direct-to-consumer advertisements continue to use this simplistic equation to ‘explain’ to a lay, non-expert audience what for the neuroscientist is still an unresolved, complex scientific question.
41
In 2012, the pharmaceutical company GlaxoSmithKline was heavily fined for having bribed doctors to continue to endorse and prescribe to children and teenagers the antidepressant Paxil (paroxetine), even though trials had shown it was only effective in adults, and its use in groups of younger individuals had been linked to risk of suicide.
42
• • •
In February 2008, producers and consumers of antidepressants were taken aback when a scientific report called into question the efficacy of antidepressants. The report surveyed a large set of data from clinical trials – including unpublished data – submitted to the US Food and Drug Administration to obtain approval for the most common SSRIs. The data were comparisons between the effects of pills and placebo on depression patients. In a nutshell, the report concluded that the prescription drugs were no better than placebo in treating those patients who manifested only mild-to-moderate depression.
43
The results were greeted with dismay especially among those for whom the drugs in question were essential bearers of comfort and the only support for a functional existence. It sounded as if they had been taking medications which in fact were no better than a sugar pill. Indeed, in the past five years or so, some of the large pharmaceutical companies have reduced their investment in mental health pharmacology and are looking for new prospects.
44
Exactly where on the scale of depressive symptoms it becomes appropriate to prescribe medication for a patient remains a controversial question just as is the choice between diagnosing or not. Not for one minute do I want to say that antidepressants never work or that they should not be prescribed. It’s obvious that some people greatly benefit from them. However, consumption figures indicate that they are prescribed way too easily – and a specific diagnosis for grief is unlikely to counteract this trend. What we should bear in mind about depression is that there is more to it than the metabolism of serotonin. It is worth pursuing the search for new medications involving different molecules and other neurochemical pathways.
45
Treatments, old and new
When I walk on the beach along the Sicilian coast where I grew up, especially when no one is around, I often think of who might have paced the same shore millennia ago. This corner of the world has been a crossroads of many and great civilizations, the stage for many wars, but also the cradle of great ideas and magnificent art. Not far from where I walk must have strode Archimedes, the mathematician and original thinker most famous for his exclamation ‘Eureka!’, or ‘I have found it!’ – which is now inevitably brought out again each time someone has a great idea.
