Pediatric Examination and Board Review (251 page)
Read Pediatric Examination and Board Review Online
Authors: Robert Daum,Jason Canel

FIGURE 142-4
A magnified view via slit-lamp biomicroscopy shows classic terminal bulbs pathognomonic for ocular HSV infection. (Reproduced, with permission, from Knoop KJ, Stack LB, Storrow AS, et al. Atlas of Emergency Medicine, 3rd ed. New York: McGraw-Hill; 2010:47. Photo contributor: Department of Ophthalmology, Naval Medical Center, Portsmouth, Virginia.)
13.
(B)
Ptosis, conjunctival injection, and discharge would be common in both periorbital and orbital cellulitis. Limited eye movement, proptosis, pupil abnormality, and/or vision loss suggest an orbital process.
14.
(E)
Conjunctival redness suggests ocular surface involvement, such as is seen with conjunctivitis, not tear duct obstruction. Redness and maceration of the eyelid skin, however, are common in tear duct obstruction due to prolonged skin contact with water and mucus. Infection in the tear sac is common with tear duct obstruction, and digital pressure on the tear sac may cause discharge to express from the puncta.
15.
(D)
The only symptom here characteristic of tear duct obstruction is tearing. Cataract and retinal detachment would produce none of these symptoms. Metabolic disease could produce all of these symptoms except corneal enlargement; additionally, the eye involvement would be bilateral. The symptoms are classic for early-onset glaucoma, which can be unilateral or bilateral.
16.
(A)
The case describes Horner syndrome (see
Figure 142-5
). In an infant, important associations are brachial plexus injury and neuroblastoma arising in the neck/upper chest area.

FIGURE 142-5
Congenital Horner syndrome. Ptosis, miosis, and heterochromia. Lighter colored iris is on the affected left side. (Reproduced, with permission, from Hay Jr WW, Levin MJ, Sondheimer JM, et al. Current Diagnosis & Treatment: Pediatrics, 19th ed. New York: McGraw-Hill; 2009: 430.)
17.
(D)
Uveitis (iritis) sometimes develops in juvenile idiopathic arthritis and is often a “silent disease,” with no early complaints of redness, photophobia, floaters, or blurred vision.
18.
(C)
The decision to treat an infant for retinopathy of prematurity is most commonly reached when the infant develops engorgement and tortuosity of the retinal blood vessels surrounding the optic nerve. Retinal detachment is generally considered a late finding, and laser treatment is ideally performed before its development. Glaucoma and cataract are not features of this disease, except when they occur as complications of cryo or laser therapy.
19.
(D)
Optic nerve hypoplasia is sometimes associated with midline central nervous system defects, such as absence of the septum pellucidum. In septo-optic dysplasia (de Morsier syndrome), pituitary abnormalities may be present.
20.
(C)
Hemangioma of the eyelid may lead to amblyopia due to occlusion of the visual axis by the tumorous eyelid or deformation of the eyeball (induced astigmatism) by the mass.
21.
(E)
A swollen optic nerve would not alter the red reflex; a cataract or a retinal tumor would.
22.
(D)
Lisch nodules are dome shaped, usually tan hamartomatous lesions of the iris surface. They are extremely common in neurofibromatosis type 1, their presence increases with age, and they are nearly universally seen in this disease by adulthood.
23.
(C)
Glaucoma is a classic ocular complication of Sturge-Weber syndrome, and children with SturgeWeber syndrome should be screened for its development (see
Figure 142-6
).
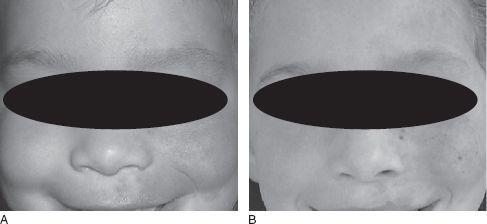
FIGURE 142-6
A girl with a large trigeminal (V1/V2) port wine stain.
A.
Appearance at age 3 years; neither glaucoma nor hypertrophy have yet developed; magnetic resonance imaging did not show Sturge-Weber syndrome.
B.
At age 5 years, after six pulsed dye laser and one alexandrite laser treatment to the affected face, labia, and oral mucosa under general anesthesia. The lesion is nearly gone. (Reproduced, with permission, from Wolff K, Goldsmith LA, Katz SI, et al. Fitzpatrick’s Dermatology in General Medicine, 7th ed. New York: McGraw-Hill; 2008: Fig. 173-4A,B.)
24.
(A)
A nonround pupil suggests the possibility that the eye was penetrated by the pencil, leading to iris and intraocular damage. Eye redness and corneal abrasion would be less serious concerns.
 S
S
UGGESTED
R
EADING
Wright K.
Pediatric Ophthalmology for Primary Care.
Elk Grove Village, IL: American Academy of Pediatrics; 2008.
Chapter 19
DENTISTRY
CASE 143: A 4-YEAR-OLD WITH DENTAL TRUAMA
DENTAL TRUAMA
The mother of a previously healthy 4-year-old girl calls your office and reports that her daughter had an accident while playing in the backyard. The child was running and fell to the ground hitting her face on the concrete. Mom reports no loss of consciousness, but the child is in pain and is crying. One of her front teeth has been “knocked out,” and they have the tooth. She has no drug allergies.
SELECT THE ONE BEST ANSWER
1.
What would be the age-appropriate number of erupted teeth for a normally developed child at age 4 years?
(A) 8
(B) 12
(C) 20
(D) 24
(E) 32
2.
What should you instruct the mother to do with the “knocked-out” tooth?
(A) place the tooth in milk and seek care at the nearest emergency department (ED)
(B) replant the tooth as soon as possible and seek care at the nearest ED
(C) discard the tooth; it should not be saved
(D) place the tooth in a buccal vestibule for safekeeping and go to the nearest ED as soon as possible
(E) place the tooth in tap water and seek care at the nearest ED
3.
If in the same scenario, the mother reports that no teeth have been “knocked out,” but the webbing inside the mouth extending from between the two middle top front teeth is “bleeding like crazy.” What should the mother be instructed to do?
(A) go to the nearest ED
(B) apply a compress to the area until the bleeding has stopped
(C) have the mother bring the child to the office immediately
(D) have the child rinse her mouth with peroxide
(E) none of the above
4.
If the child’s age is 9 years, in the same scenario, and the mother reports that an upper middle tooth has been “knocked out,” what should the mother be instructed to do with the tooth?
(A) replant the tooth in the socket immediately and go to the ED or the dentist
(B) place the tooth in milk and go to the ED or the dentist
(C) store the tooth in a warm dark environment (ie, pants pocket) and go to the ED or the dentist
(D) do nothing with the tooth; it should not be saved
(C) place the tooth in tap water and go to the ED or the dentist
5.
The patient has had a tooth splinted by a dentist on call at the ED and has come to your office immediately afterward for follow-up. The antibiotic of choice would be which one of the following?
(A) amoxicillin
(B) clindamycin
(C) doxycycline
(D) phenoxymethyl penicillin (penicillin V)
(E) no antibiotic is indicated; the tooth is not infected
6.
A 2-year-old boy comes to your office for a routine physical examination. You notice a dark-colored front primary tooth. He is in no pain and the parent does not care if it is discolored. What would be the appropriate next step?
