Pediatric Primary Care Case Studies (84 page)
Read Pediatric Primary Care Case Studies Online
Authors: Catherine E. Burns,Beth Richardson,Cpnp Rn Dns Beth Richardson,Margaret Brady
Tags: #Medical, #Health Care Delivery, #Nursing, #Pediatric & Neonatal, #Pediatrics

Rubin, D. H., Suecoff, S. A., & Knupp, K. (2006). Headaches in children.
Pediatric Annals, 35
(5), 345–353.
Vannetta, K., Getzoff, E. A., Gilman, D. K., Noll, R. B., Gerhardt, C. A., Powers, S. W., et al. (2008). Friendships and social interactions of school-aged children with migraine.
Cephalalgia, 28
, 734–743.
Chapter 21
The Preschooler with a Red Eye
Michele Saysana
In many encounters in medicine, tests exist to confirm the diagnosis; however, the test results may not be readily available, thus leaving the practitioner to make a diagnosis as well as treatment recommendations based on the history and physical alone. By putting together the signs and symptoms based on the history and physical exam, the practitioner is able to make a diagnosis and treatment plan without the confirmatory test.
Educational Objectives
1. Identify the distinguishing signs and symptoms of bacterial, viral, and allergic conjunctivitis.
2. Discuss the different treatments of bacterial, viral, and allergic conjunctivitis.
3. Identify when patients need to be referred to an ophthalmologist for treatment of conjunctivitis.
Case Presentation and Discussion
Jack Cho is a 5-year-old Asian American boy who presents to your office because he was sent home from school today by the school nurse who said he had “pink eye.” He is accompanied by his pregnant mother and his 19-month-old sister.
You talk with Jack and his mother about his symptoms and plan to complete a physical examination.
What questions will you ask Jack and his mother related to his “pink eye”?
Your symptom analysis reveals the following information: He woke up this morning with a crusted shut right eye. After his mother applied a warm washcloth to his face, the crusting disappeared. He had more yellow drainage out of his right eye while on the bus to school. He continued to have yellow drainage and a red eye at school, so his teacher sent him to the school nurse. He states his eye is not itchy or burning. Jack and his mother do not recall any trauma to the eye. Jack does not have any cough, rhinorrhea, fever, or ear or throat pain. He does not have any history of allergic rhinitis either. Upon further questioning, he tells you other children have been sent home from his class for “pink eye” this week, including the boy who sits next to him.
What other questions do you need to ask Jack?
Before answering this question, here is some more information about “pink eye” that you need to consider.
Information about “Pink Eye”
Epidemiology
Conjunctivitis is the most common pediatric eye disorder that primary care practitioners will encounter (Wald, 2004). In developed countries worldwide, acute bacterial or viral conjunctivitis has an annual incidence in adults and children of 1.5–2%, with one in eight school-age children affected each year (Rietveld, ter Riet, Bindels, Sloos, & van Weert, 2004; Rose et al., 2005). Bacterial pathogens account for 54–73% of conjunctivitis, with nontypable
Haemophilus influenzae
and
Streptococcus pneumoniae
as the most common bacterial pathogens (Buznach, Dugan, & Greenberg, 2005). Viral conjunctivitis can be caused by many different viruses, the most common being adenovirus (Langley, 2005). Enterovirus and influenza are also considered to be important causes of viral conjunctivitis (Pickering, Baker, Long, & McMillan, 2006).
Data for the Diagnosis
History
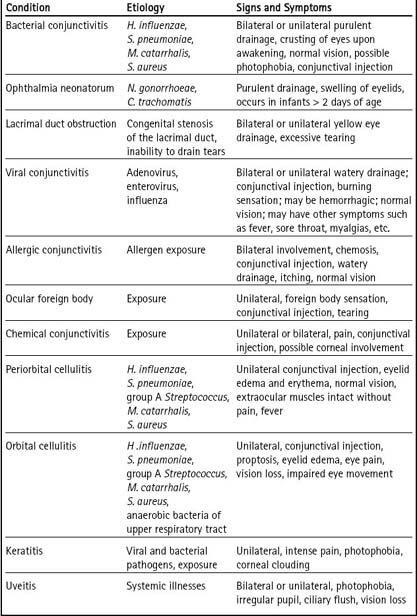
The differential diagnoses include bacterial, viral, and allergic conjunctivitis; hyperacute bacterial conjunctivitis; ophthalmia neonatorum; epidemic keratoconjunctivitis; chemical conjunctivitis; ocular foreign body; periorbital and orbital cellulitis; keratitis; uveitis; glaucoma; or possible systemic disease processes such as Kawasaki disease, Stevens-Johnson syndrome, juvenile idiopathic arthritis, inflammatory bowel disease, or lupus. (See
Table 21-1
.)
In this situation, the information that needs to be gathered includes the following:
• How old is the patient? (Certain causes for conjunctivitis are included and excluded based on age.)
• Is there drainage from the eye, what color, and how much? (Helps to distinguish among bacterial, viral, and allergic conjunctivitis, as well as hyperacute bacterial conjunctivitis and some of the systemic causes of red eye)
• Is the drainage persistent and yellow in color? (Bacterial conjunctivitis)
• Is the drainage watery in nature? (Viral conjunctivitis, allergic conjunctivitis)
• Does the patient wake up with the affected eye matted shut due to discharge? (Bacterial conjunctivitis)
• Is there associated itching of the eye? (Allergic conjunctivitis)
• Is the eye painful? (Keratitis, uveitis, orbital cellulitis, foreign body)
• Is there vision loss? (Uveitis, orbital cellulitis)
• Is there photophobia? (Bacterial conjunctivitis, viral conjunctivitis, epidemic keratoconjunctivitis, uveitis, keratitis)
Table 21–1 Distinguishing Causes of Red Eye
• Does the patient wear contact lenses? (Keratitis)
• Has there been any trauma or toxin exposure to the eye? (Chemical conjunctivitis, foreign body)
• Does the patient have otitis media and conjunctivitis? (Nontypable
H. influenzae
conjunctivitis)
• Does the patient have associated symptoms such as sore throat and fever? (Viral conjunctivitis)
• Does the patient have significant swelling and erythema of the eyelids with or without proptosis? (Periorbital and orbital cellulitis, epidemic keratoconjunctivitis)
• Does the patient have clouding of the cornea? (Glaucoma, keratitis, epidemic keratoconjunctivitis)
• Does the patient have a nonpurulent conjunctivitis associated with fever for at least 5 days, perineal diaper rash, pharyngitis, strawberry tongue, or cervical lymphadenopathy? (Kawasaki disease)
• Does the patient have associated symptoms suggesting a systemic illness such as fever, weight loss, diarrhea, or arthritis? (Juvenile idiopathic arthritis, inflammatory bowel disease, lupus)
• Does the patient have associated symptoms such as bullae of skin and aphthous ulcers of oral mucosa? (Stevens-Johnson syndrome)
Physical Examination
Data from your physical examination will give you the remaining information that you need to make a reasonable diagnosis.
Upon physical examination, Jack is nontoxic in appearance and cooperative with your exam. His right eyelid margin and corners of his eye have purulent yellow discharge. His right eye has an injected, red conjunctiva. His left eye is normal without discharge or conjunctival injection. He has 20/20 vision in both eyes. His pupils are both equal and reactive to light and his extraocular muscles are intact without any pain upon movement of either eye. He does not have any photophobia. His ear exam is normal without any bulging or erythema of his tympanic membranes. Examination of his nose does not reveal any bogginess of the mucosa or nasal drainage. His oropharynx is normal without any erythema or cobblestoning. He does not have any lymphadenopathy.
Making the Diagnosis
This history and physical examination are consistent with a diagnosis of bacterial conjunctivitis. The combination of crusted eyelid in the morning, a red eye, and purulent discharge on physical exam are indicative of bacterial conjunctivitis (Patel, Diaz, Bennett, & Attia, 2007). Acute infectious conjunctivitis is defined as conjunctival injection with eye discharge (Wald, 2004); however, there are multiple causes of a red eye that must be included in the differential diagnosis of conjunctivitis.
Differential Diagnosis
Usually the diagnosis of conjunctivitis is not complicated and is based on the history and physical examination findings. The history and physical examination are important to help guide one down the right path on the differential diagnosis. When evaluating a patient with suspected conjunctivitis, the healthcare provider needs to consider the following characteristic clinical findings to point to the causative agent.
Bacterial conjunctivitis is usually characterized by unilateral injected conjunctiva, purulent drainage, and matted eye upon awakening, and is most commonly caused by either nontypable
H. influenzae
or
S. pneumoniae
(Patel et al., 2007). Bacterial conjunctivitis due to
H. influenzae
may also be present with otitis media. Infants may also have lacrimal duct stenosis, which can present with unilateral or bilateral yellow drainage and is often confused with conjunctivitis. Usually the conjunctiva is not injected, and the drainage will often persist despite the use of topical ophthalmic antibiotic drops. Ophthalmia neonatorium occurs in infants less than 1 month of age and is usually due to
Neisseria gonorrhoeae
or
Chlamydia trachomatis.
It is acquired during vaginal delivery by a mother who is infected with
N. gonorrhoea
or
C. trachomatis
as a sexually transmitted infection. It is characterized by purulent drainage from the eye after 48 hours of life (Olitsky, Hug, & Smith, 2007). Older children, especially adolescents, may also develop an acute purulent conjunctivitis secondary to infection with
N. gonorrheae
or
C. trachomatis.
Viral conjunctivitis is often characterized by watery discharge, burning, itching, and injection of the conjunctiva. Conjunctivitis due to adenovirus may also be associated with pharyngitis and fever called pharyngoconjunctival fever. Outbreaks have occurred in contaminated swimming pools and ponds. Adenovirus can also lead to epidemic keratoconjunctivitis, which usually is characterized by conjunctivitis with a foreign body sensation, discharge, photophobia, itching, burning, edema of the lid, and associated upper respiratory infection (URI) symptoms. Outbreaks have occurred in ophthalmology offices and neonatal intensive care units (Langley, 2005). Acute hemorrhagic conjunctivitis, caused by enterovirus, includes symptoms such as watery hemorrhagic discharge with painful eyes (Pickering et al., 2006; Olitsky et al., 2007). Influenza infection may also lead to conjunctivitis, which is often associated with sudden onset of fever, malaise, sore throat, myalgias, and cough and has a seasonal epidemic period in the winter months (Pickering et al.).

