Resident Readiness General Surgery (76 page)
Read Resident Readiness General Surgery Online
Authors: Debra Klamen,Brian George,Alden Harken,Debra Darosa
Tags: #Medical, #Surgery, #General, #Test Preparation & Review

Roy Phitayakorn, MD, MHPE (MEd)
A 35-year-old woman presents to general surgery resident clinic with a 3 × 4 cm soft tissue mass on her upper back that she would like to have removed. She states that the mass has been there for several years, but recently started growing after she hit that portion of her back on a door. The mass is soft and mobile and pictured in
Figure 58-1
. Her lymph nodes are all normal and the mass feels like a lipoma.

Figure 58-1.
A picture of a lipoma that was removed in clinic under local anesthetic.
1.
What are the 2 main classes of local anesthetics?
2.
What is the mechanism of action of local anesthetics?
3.
Where in the body is local anesthetic mixed with epinephrine contraindicated?
4.
What is the most serious risk of using local anesthetics?
5.
Name 2 things you can do to minimize the pain associated with injection of local anesthetics.
6.
How many distinct skin injections are required for a small field block?
LOCAL ANESTHETICS
Answers
1.
Local anesthetics can be separated into 2 distinct groups called amides or esters based on their chemical structures. All anesthetics that end in “-caine” and contain the letter i in the prefix are amide agents. An easy way to remember this for the ABSITE is that the word amide also has an “i” in it. So, for example, lido-caine is an amide and cetacaine is an ester. Esters have the advantage of being faster acting. The disadvantages of ester anesthetics are that they have a shorter shelf life and cannot be combined with epinephrine.
2.
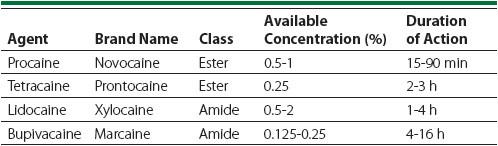
Remember from your preclinical years that pain signals are transmitted via action potentials along the peripheral nerves. Local anesthetics act by reversibly blocking these nerve impulses by disrupting cell membrane permeability to sodium during an action potential. The basic pharmacokinetics of common local anesthetics is illustrated in
Table 58-1
. The 2 most common local anesthetics general surgery residents use are lidocaine (Xylocaine
®
) and bupivacaine (Marcaine
®
). Both take several minutes to take effect after injection and last anywhere from several hours in the case of lidocaine to many hours for bupivacaine.
Table 58-1.
Common Local Anesthetics
The most important detail to remember when using these agents is to keep track of the total amount of anesthetic given. This is especially important when
you may be suturing by yourself in the emergency department on a patient with multiple lacerations. If you think you will need a lot of local anesthetic due to multiple lacerations, then the 1% concentration of lidocaine (10 mg/mL) or 0.5% bupivacaine (5 mg/mL) is a convenient choice. For an average patient with no hepatic impairment, up to 4.5 mg/kg of lidocaine or 2.5 mg/kg of bupiva-caine can be given during the procedure.
3.
Epinephrine is combined with these anesthetics in various concentrations and helps to promote vasoconstriction of nearby vessels. This provides several benefits including lower required dosages of anesthetic, prolonged duration of action, and improved control of local bleeding. Local anesthetic with epinephrine is contraindicated in areas of the body with end arterioles. These
anatomical areas are easily remembered by the rhyme “No epinephrine in the fingers, nose, toes, ear lobes, and ‘hose.’”
4.
There are several problems that you may encounter when using local anesthetics. One problem is systemic toxicity, which frequently manifests first as central nervous system–type symptoms such as confusion, dizziness, tinnitus, somnolence, and possible seizures. These symptoms can eventually progress if unrecognized to cardiovascular collapse, ventricular arrhythmias, and asystole due to a direct blocking effect on cardiac and vascular smooth muscle. Treatment is mainly supportive until the anesthetic has been metabolized. Pregnant patients are a special case in terms of local anesthetics as pregnancy reduces the risk of toxicity, but much higher dosages of the local anesthetics are required to achieve effective anesthesia. The mechanism for this tolerance is not clearly understood.
5.
There are 5 things you can do to minimize the pain of injection: buffering, medications for anxiety, use a small needle, inject slowly, and wound pretreatment.
Buffering:
Local anesthetic is an acidic solution and therefore creates a burning sensation when you inject it into the skin. Anyone who has not experienced the feeling of lidocaine should definitely try it before one tells a patient “This won’t hurt a bit.” There are several proven techniques to reduce the pain of injection. One technique is to use sodium bicarbonate, which buffers the acidic solution so that it does not burn as much. Generally, you use the bicarbonate in a 1:10 ratio for 1% lidocaine and 2:10 for 2% lidocaine. It used to be believed that buffering lidocaine increased the rate of infection in contaminated wounds, but this was found to be untrue in experimental models. However, the use of bicarbonate does decrease the shelf life of lidocaine considerably so you should generally use whatever you mix. Also, when you ask for lidocaine from the inpatient pharmacy, it may have been stored in a refrigerator to preserve shelf life. It is important to warm the solution to body temperature if possible as cold lidocaine is more painful for the patient on injection than room-temperature lidocaine.
Medications for anxiety:
Another important technique to minimize pain associated with local anesthetics is to remember the old cliché that “perception is reality” and that local anesthetics do not do anything for patient anxiety. If the patient is particularly anxious, he or she may benefit from a preprocedure injection of opioids or anxiolytics before you inject the anesthetic as a way to decrease overall receptiveness to pain. Common choices are fentanyl or morphine and Ativan or Versed. Fentanyl and Versed work faster if you are ready to start the procedure, but may be more difficult to obtain quickly.
Use a small needle:
Although it is quicker to draw up the lidocaine using an 18- or 20-gauge needle, you should inject with the smallest needle possible. Nothing stimulates anxiety like watching someone approach you with a large needle.
Inject slowly:
You should also strive to inject the local anesthetic slowly into the skin as this allows the tissue to slowly expand and decreases pain. A good rule of thumb is 1 mL of local anesthetic over 5 seconds of time. You should also try to inject local anesthetic through areas of the skin that are already anesthetized.
Wound pretreatment:
The last technique to minimize pain is the most complicated and is in the broad category of wound pretreatment. One type of wound pretreatment is distraction. Mechanical distraction is a very interesting, but poorly understood phenomenon. Likely the mechanism is that your peripheral nerves can only carry so much sensory information at a given time. A good use of this technique is when you need to start peripheral IVs. If you take your skin and pinch it hard, you will notice after you let go that the area is slightly numb. Similarly, stretching the skin around a wound while injecting local anesthetic seems to decrease the perception of pain. Psychological distraction works on the belief that anxiety may play a large role in the perception of pain, especially in children. Therefore, for adult patients, try to engage them in conversation to keep them occupied. For pediatric patients, try to use child life specialists if possible to provide age-appropriate distracters such as blowing bubbles, music, or videos.
Another form of wound pretreatment is thermal anesthesia. A clean piece of ice or ice pack on top of a wound for at least 10 seconds is very effective at decreasing pain. A chemical version is ethyl chloride (also called Pain-eze
®
), as it functions to cool the skin and thus decrease pain perception. If you do use ethyl chloride, you have to be very careful to spray only for a few seconds as prolonged exposure to ethyl chloride can cause frostbite on the skin.
The last common form of wound pretreatment is EMLA cream, which is predominantly used in the pediatric population. EMLA stands for eutectic mixture of local anesthetics. As the chemistry majors who are reading this may remember, a eutectic mixture is a mixture of 2 substances that has a melting point lower than either substance by itself. In EMLA cream, the crystalline bases of lidocaine and prilocaine are combined to produce a liquid at room temperature. The cream is applied to an area and covered with occlusive dressing. Onset time is 15 minutes, but requires 1 hour to penetrate the first 3 mm of skin. One common fear is toxicity, but the literature suggests that systemic toxicity is very unlikely. Generally you should use enough so that you still see residual cream when you remove the occlusive dressing.
6.
A useful technique when removing soft tissue masses such as a lipoma or an epidermoid inclusion cyst is illustrated in
Figure 58-2
. First, inject anesthetic at 2 points across the mass from each other. Once these areas are anesthetized,
inject local anesthetic through these points to form a rectangle around the mass. Remember, the goal is to inject the local anesthetic into the deep dermis (
not
the subcutaneous fat or the epidermis) to block the sensory plexus. This technique is called a field block and essentially completely disrupts the ability to send any pain signals out of the area where you will be dissecting, and yet only requires 2 skin injections.
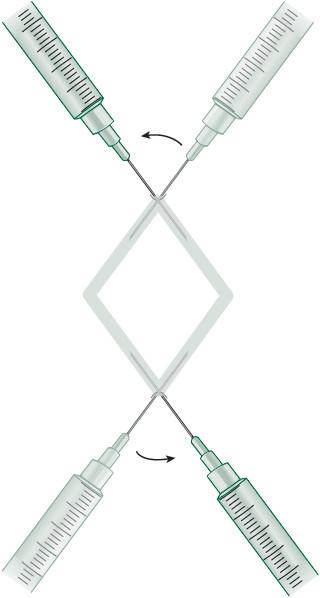
Figure 58-2.
The field block technique.
TIPS TO REMEMBER
Lidocaine and bupivacaine are the most commonly used local anesthetics for general surgery problems.
