Ross & Wilson Anatomy and Physiology in Health and Illness (42 page)
Read Ross & Wilson Anatomy and Physiology in Health and Illness Online
Authors: Anne Waugh,Allison Grant
Tags: #Medical, #Nursing, #General, #Anatomy

Stroke volume
The stroke volume is determined by the volume of blood in the ventricles immediately before they contract, i.e. the ventricular end-diastolic volume (VEDV), sometimes called
preload
. In turn, preload depends on the amount of blood returning to the heart through the superior and inferior venae cavae (the
venous return
). Increased preload leads to stronger myocardial contraction, and more blood is expelled. In turn the stroke volume and cardiac output rise. In this way, the heart, within physiological limits, always pumps out all the blood that it receives, allowing it to adjust cardiac output to match body needs. This capacity to increase the stroke volume with increasing preload is finite, and when the limit is reached, i.e. venous return to the heart exceeds cardiac output (i.e. more blood is arriving in the atria than the ventricles can pump out), cardiac output decreases and the heart begins to fail (
p. 119
). Other factors that increase myocardial contraction include:
•
increased sympathetic nerve activity to the heart
•
hormones, e.g. adrenaline (epinephrine), noradrenaline (norepinephrine), thyroxine.
Arterial blood pressure
This affects the stroke volume as it creates resistance to blood being pumped from the ventricles into the great arteries. This resistance (sometimes called
afterload
) is determined by the distensibility, or
elasticity
, of the large arteries and the peripheral
resistance
of arterioles. Increasing afterload increases the workload of the ventricles, because it increases the pressure against which they have to pump. This may actually reduce stroke volume if systemic blood pressure becomes significantly higher than normal.
Blood volume
This is normally kept constant by the kidneys. Should blood volume fall, e.g. through sudden haemorrhage, this can cause stroke volume, cardiac output and venous return to fall. However, the body’s compensatory mechanisms (
p. 88
) will tend to return these values towards normal, unless the blood loss is too sudden or severe for compensation (see
Shock, p. 111
).
Venous return
Venous return is the major determinant of cardiac output and, normally, the heart pumps out all blood returned to it. The force of contraction of the left ventricle ejecting blood into the aorta is not sufficient to push the blood through the arterial and venous circulation and back to the heart. Other factors are involved.
The position of the body
Gravity assists venous return from the head and neck when standing or sitting and offers less resistance to venous return from the lower parts of the body when an individual is lying flat.
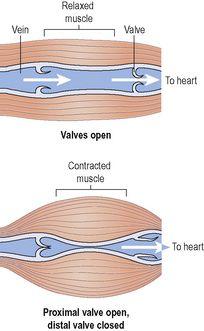
Muscular contraction
Backflow of blood in veins of the limbs, especially when standing, is prevented by valves (
Fig. 5.4
). The contraction of skeletal muscles surrounding the deep veins compresses them, pushing blood towards the heart (
Fig. 5.23
). In the lower limbs, this is called the
skeletal muscle pump
.
Figure 5.23
The skeletal muscle pump.
The respiratory pump
During inspiration, the expansion of the chest creates a negative pressure within the thorax, assisting flow of blood towards the heart. In addition, when the diaphragm descends during inspiration, the increased intra-abdominal pressure pushes blood towards the heart.
Heart rate
The heart rate determines cardiac output. If heart rate rises, cardiac output increases, and if it falls, cardiac output falls too. The main factors determining heart rate are outlined below.
Autonomic nervous system
The intrinsic rate at which the heart beats is a balance between sympathetic and parasympathetic activity and this is the most important factor in determining heart rate.
Circulating chemicals
The hormones adrenaline (epinephrine) and noradrenaline (norepinephrine), secreted by the adrenal medulla, have the same effect as sympathetic stimulation, i.e. they increase the heart rate. Other hormones, including thyroxine, increase heart rate by their metabolic effect. Hypoxia and elevated carbon dioxide levels stimulate heart rate. Electrolyte imbalances may affect it, e.g. hyperkalaemia depresses cardiac function and leads to bradycardia (slow heart rate). Some drugs, such as β-receptor antagonists (e.g. atenolol) used in hypertension, can also cause bradycardia.
Position
When the person is upright, the heart rate is usually faster than when lying down.
Exercise
Active muscles need more blood than resting muscles and this is achieved by an increased heart rate and selective vasodilation.
Emotional states
During excitement, fear or anxiety the heart rate is increased. Other effects mediated by the sympathetic nervous system may be present (see
Fig. 7.46, p. 168
).
Gender
The heart rate is faster in women than men.
Age
In babies and small children the heart rate is more rapid than in older children and adults.
Temperature
The heart rate rises and falls with body temperature.
Baroreceptor reflex
See
page 88
.
A summary of the factors that alter CO is shown in
Box 5.2
.
Blood pressure
Learning outcomes
After studying this section, you should be able to:
define the term blood pressure
describe the main control mechanisms for regulation of blood pressure.
Blood pressure is the force or pressure that the blood exerts on the walls of the blood vessels. Systemic arterial blood pressure maintains the essential flow of blood into and out of the organs of the body. Keeping blood pressure within normal limits is very important. If it becomes too high, blood vessels can be damaged, causing clots or bleeding from sites of blood vessel rupture. If it falls too low, then blood flow through tissue beds may be inadequate. This is particularly dangerous for such essential organs as the heart, brain or kidneys.
The systemic arterial blood pressure, usually called simply arterial blood pressure, is the result of the discharge of blood from the left ventricle into the already full aorta.
Blood pressure varies according to the time of day, the posture, gender and age of the individual. Blood pressure falls at rest and during sleep. It increases with age and is usually higher in women than in men.
Systolic and diastolic pressure
When the left ventricle contracts and pushes blood into the aorta, the pressure produced within the arterial system is called the
systolic blood pressure
. In adults it is about 120 mmHg or 16 kPa.
When
complete cardiac diastole
occurs and the heart is resting following the ejection of blood, the pressure within the arteries is much lower and is called
diastolic blood pressure
. In an adult this is about 80 mmHg or 11 kPa. The difference between systolic and diastolic blood pressures is the
pulse pressure
.
Arterial blood pressure is measured with a
sphygmomanometer
and is usually expressed with the systolic pressure written above the diastolic pressure:
Elasticity of arterial walls
There is a considerable amount of elastic tissue in the arterial walls, especially in large arteries. Therefore, when the left ventricle ejects blood into the already full aorta, the aorta expands to accommodate it, and then recoils because of the elastic tissue in the wall. This pushes the blood forwards, into the systemic circulation. This distension and recoil occurs throughout the arterial system. During cardiac diastole the elastic recoil of the arteries maintains the diastolic pressure (
Fig. 5.21
).