Pediatric Examination and Board Review (234 page)
Read Pediatric Examination and Board Review Online
Authors: Robert Daum,Jason Canel

(A) migraine with aura (classic migraine)
(B) complex partial seizure
(C) basilar artery migraine
(D) ophthalmoplegic migraine
(E) complicated migraine
10.
An 18-year-old young man presents to the ED with the chief complaint of headache. He has had occasional headaches before this one but states, “this is the worst headache of my life.” On the way to the ED, the patient complained of nausea and vomited. He now complains of pain on flexing his head forward. The patient is afebrile. The next most appropriate action is which of the following?
(A) order a head CT
(B) perform a lumbar puncture
(C) administer an opiate analgesic agent, such as morphine
(D) order a urine toxicology screen
(E) assure the patient that this is probably a migraine, which will get better
11.
The radiology resident for the patient in question 10 calls you to tell you that the head CT is probably normal. With this information, you next decide to perform a spinal tap, which reveals a yellow fluid with occasional red blood cells. This patient most likely has which of the following diagnoses?
(A) complicated migraine
(B) herpes simplex hemorrhagic meningoencephalitis
(C) acute subdural hematoma
(D) subarachnoid hemorrhage
(E) glioblastoma multiforme
12.
Which of the following drugs are used as prophylactic agents in the treatment of migraine headaches?
(A) cyproheptadine
(B) valproic acid
(C) amitriptyline
(D) propranolol
(E) all of the above
13.
Hemicrania continua is especially responsive to which of the following medications?
(A) ibuprofen
(B) sumatriptan
(C) cyproheptadine
(D) indomethacin
(E) none of the above
14.
Sumatriptan is an example of which of the following categories of medications used in the treatment of migraines?
(A) antidepressant
(B) beta-blocker
(C) 5-HT receptor agonist
(D) antiepileptic drug
(E) nonsteroidal anti-inflammatory agent
15.
Which of the following are typical triggers of migraine headaches?
(A) menstruation
(B) stress
(C) cheese
(D) fatigue
(E) all of the above
16.
Which of the following primary brain tumors is the most common type encountered in children younger than 15 years of age?
(A) meningioma
(B) supratentorial low-grade astrocytoma
(C) medulloblastoma
(D) ependymoma
(E) cerebellar astrocytoma
17.
A 3-year-old boy presents to the ED with a 3-month history of headache, nausea, and vomiting. The patient has progressively gotten worse and now is ataxic.
Figure 136-1
shows an MRI of his brain. Based on this information, this patient most likely has which of the following posterior fossa brain tumors?
(A) cerebellar astrocytoma
(B) medulloblastoma
(C) ependymoma
(D) brainstem glioma
(E) meningioma
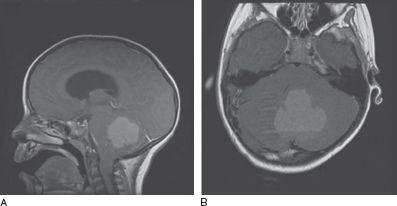
FIGURE 136-1
.
A brain MRI of a 3-year-old boy presenting with headache, nausea, and vomiting from question 17. (
A
) Sagittal T1-weighted image following contrast administration. (
B
) Axial T1-weighted image. (Courtesy of Dr. Daniel Curry, University of Chicago.)
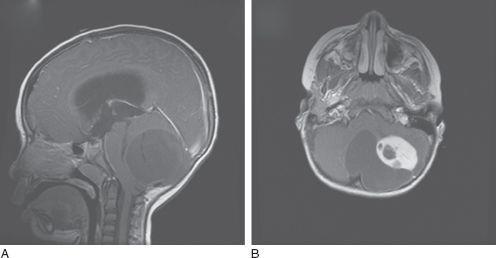
FIGURE 136-2
.
A brain MRI of a 4-year-old boy presenting with headache, nausea, and vomiting from question 18. (
A
) Sagittal T1-weighted image following contrast administration. (
B
) Axial T1-weighted image following contrast administration. (Courtesy of Dr. Daniel Curry, University of Chicago.)
18.
On the same night you see a 4-year-old boy who presents to the ED with similar symptoms. He has a 3-month history of progressive headaches, nausea, vomiting, and ataxia. His ataxia is so severe that he no longer is able to walk. He was recently seen by his primary physician who treated him with antibiotics for an otitis media without resolution of his symptoms. His MRI of the brain is shown in
Figure 136-2
. This patient most likely has which of the following diagnoses?
(A) cerebellar astrocytoma
(B) medulloblastoma
(C) ependymoma
(D) brainstem glioma
(E) meningioma
19.
A 2-year-old girl presents to the ED with inconsolable crying and vomiting. An MRI of the brain and a head CT are shown in
Figure 136-3
. The most likely cause(s) of this patient’s symptoms is which of the following?
(A) choroid plexus papilloma
(B) subependymal giant cell astrocytoma
(C) hydrocephalus
(D) colloid cyst
(E) A and C are correct
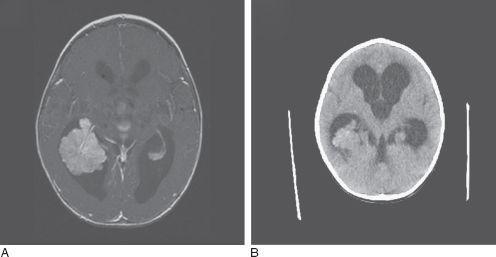
FIGURE 136-3
.
A brain MRI and head CT of a 2-year-old girl presenting with inconsolable crying and vomiting from question 19. (A) Sagittal T1-weighted image following contrast administration. (B) Head CT. (Courtesy of Dr. Daniel Curry, University of Chicago.)
ANSWERS
1.
(A)
In a patient who presents with headache and papilledema, it is important to rule out hydrocephalus or a mass lesion given the potential of developing a herniation syndrome. In fact, in this case neuroimaging is mandatory before performing a lumbar puncture. Although an MRI of the brain with and without contrast is the preferred study, especially if the practitioner suspects meningeal disease, a head CT with contrast can be useful. In fact, the head CT may be more readily available and the only option if the patient is extremely obese (other than an open MRI). In addition, a head CT would be very helpful in evaluating an intracerebral hemorrhage. For postpartum patients or those on oral contraceptives, MRI has the added advantage of being able to perform a magnetic resonance venogram (MRV) to rule out cerebral venous thrombosis. Once a structural lesion and hydrocephalus are ruled out, a lumbar puncture can be performed. Tonometry is used to measure intraocular pressure as part of an evaluation for glaucoma. Although visual field testing is a sensitive tool in assessing optic nerve involvement, the test would be performed following a neuroimaging study done to define the cause of the papilledema.
2.
(E)
In evaluating a patient with papilledema, it is important to look for an underlying cause. Several medical conditions are associated with papilledema. These include neurologic conditions, such as CNS tumors (primary and metastatic), infectious conditions, medications and toxins, such as tetracycline, vitamin A, and lead, certain endocrine diseases, autoimmune diseases, such as lupus erythematous, vascular diseases; and hematologic diseases.
3.
(D)
The study most likely to yield the diagnosis in this patient is the lumbar puncture to measure opening pressure. To accurately assess visual function in patients with papilledema, perimetry, either by Goldmann field testing or by the static Humphrey method, should be performed. In the case of papilledema, an enlargement of the blind spot is typically seen. Although perimetry is the most useful test for evaluating visual function, it does not provide the etiology for the papilledema. Vitamin A toxicity has been associated with diplopia and pseudotumor cerebri. However, one should be able to assess for vitamin A toxicity with good historytaking skills. The erythrocyte sedimentation rate is a nonspecific test for inflammation and may be elevated in patients with autoimmune conditions. If cerebral vasculitis is suspected clinically, a cerebral angiogram should be performed to assess narrowing of the blood vessels. If a venous sinus thrombosis is clinically suspected, conventional cerebral angiography should be performed, especially if noninvasive methods such as magnetic resonance angiography and computed tomography angiography are not available.
4.
(B)
The normal range of CSF pressure is 100-200 mm H
2
O. Hence a pressure of 280 mm H
2
O is elevated. Given the papilledema, normal MRI of the brain, and raised intracranial pressure as measured by lumbar puncture, this patient most likely has pseudotumor cerebri. Glaucoma, an elevation in intraocular pressure, can mimic the visual field deficit seen in pseudotumor cerebri because it can cause optic nerve damage. The normal intraocular pressure measured by tonometry rules out this diagnosis. An Arnold-Chiari type I malformation refers to cerebellum and cerebellar-tonsillar displacement 5 mm or more beyond the foramen magnum line. Patients may also have syringomyelia. Clinically, patients with Arnold-Chiari type 1 malformation complain of recurrent headaches, primarily over the frontal and occipital regions, neck pain, difficulty swallowing, and ataxia. The headaches can be exacerbated by exertion. In patients with syringomyelia, upper limb sensory changes and weakness are sometimes also observed. Arnold-Chiari type 2 malformations are similar to type 1 but are associated with myelomeningocele. A type 3 Arnold-Chiari malformation consists of the cerebellar displacement defined above and an encephalocervical meningocele. Type 4 consists of hypoplasia of the cerebellum and may actually represent a variation of a Dandy-Walker malformation. The normal MRI of the brain ruled out the Arnold-Chiari malformations. Finally, migraines and chronic daily headaches are not associated with abnormal physical findings, such as papilledema or elevated intracranial pressure.
