Resident Readiness General Surgery (23 page)
Read Resident Readiness General Surgery Online
Authors: Debra Klamen,Brian George,Alden Harken,Debra Darosa
Tags: #Medical, #Surgery, #General, #Test Preparation & Review

Antibiotic choice
: For the immunocompetent host with a simple, drained abscess and surrounding cellulitis, empiric coverage with an oral β-lactam antibiotic is appropriate to cover staphylococcal and streptococcal organisms: dicloxacillin or cephalexin (even if penicillin-allergic but without any immediate hyper-sensitivity reaction). If there is concern for MRSA (see above) or the patient has an allergy to penicillin, alternative oral antibiotic option is clindamycin or TMP-SMZ.
Patients with extensive, severe cellulitis and signs of systemic toxicity (ie, fevers, abnormal vital signs, etc) should receive parenteral antibiotics that cover MRSA as well as gram-negative and anaerobic bacteria. Two typical antibiotic regimens are:
•
Vancomycin (MRSA coverage),
and
•
Piperacillin–tazobactam
or
ticarcillin–clavulanate (gram-negative+anaerobic coverage)
Or
•
Vancomycin (MRSA coverage),
and
•
Ceftriaxone
or
ciprofloxacin (gram-negative coverage),
and
•
Metronidazole (anaerobic coverage)
Diabetics often have more severe soft tissue infections involving
Pseudomonas
. These typically require treatment with an antipseudomonal antibiotic, such as piperacillin–tazobactam or cefepime.
The patient presented here has significant surrounding cellulitis that is concerning, although he has no systemic signs of infection. A reasonable treatment plan after I&D is to start an oral antibiotic (dicloxacillin or cephalexin) and admit the patient for 12 to 24 hours to ensure improvement of the cellulitis after a day of antibiotic treatment.
TIPS TO REMEMBER
Bedside ultrasound is a useful modality for both diagnosis and procedural planning.
The length of the incision for an abscess can vary but should be large enough to ensure adequate drainage.
After incision, adequate drainage requires you to break up the loculations and loosely pack the cavity with gauze or other packing material.
Assuming an abscess is adequately drained, the main indications for antibiotic therapy are: (1) presence of surrounding cellulitis, (2) severe infection with systemic signs of illness, or (3) patient immunocompromise (eg, from diabetes).
COMPREHENSION QUESTIONS
1.
To ensure adequate drainage of a superficial abscess, which of the following is/are important component(s)? (Choose all that apply.)
A. Skin incision large enough to ensure adequate drainage
B. Deloculation of abscess cavity
C. Antibiotic treatment
D. Loose packing
2.
Which of the following are contraindications to I&D of a superficial abscess under local anesthesia? (Choose all that apply.)
A. Immunocompromised patient
B. History of injection drug use
C. Large size
D. Sensitive location
E. Location requiring extensive exposure
Answers
1.
A, B, D
. Antibiotic treatment is most important for treatment of surrounding cellulitis, not for drainage of an abscess.
2.
C, D, E
. Immunocompetency and history of drug use are risk factors for more severe infection, but do not preclude drainage of the abscess under local anesthesia.
 Three Patients All Present With Issues Related to Laboratory Tests
Three Patients All Present With Issues Related to Laboratory Tests
Abigail K. Tarbox, MD and Mamta Swaroop, MD, FACS
Case 1: Mr. Jones is a 51-year-old male who comes to your office for a screening colonoscopy. He tells you that he had a friend who had a colon perforation from a colonoscopy and he is reluctant to undergo one himself. He has heard that there is a new blood test for colon cancer and asks you why he can’t have this instead. You do a quick search for this test and learn that it has low sensitivity but high specificity.
Case 2: Mrs. Smith has been on a therapeutic heparin drip with a goal partial thromboplastin time (PTT) of 60 to 80. For the last 3 lab draws, her values have been 70, 73, and 69. Because her PTT has been at goal, you have not changed the rate of her drip. On her next set of labs her PTT suddenly becomes 133.
Case 3: Jane Doe has a urine specimen with the following results:
2 to 3 white blood cells
50,000 bacteria per high-power field
Negative nitrite
Negative leukocyte esterase
Multiple squamous epithelial cells
1.
Should you order this new blood test for Mr. Jones?
2.
What is the next step in evaluating Mrs. Smith’s newly elevated PTT?
3.
Does Jane Doe have a urinary tract infection?
LABS 101
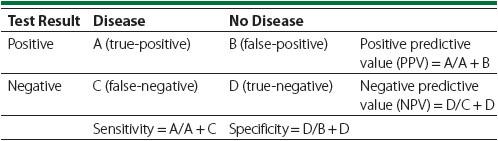
Doctors spend a significant portion of their time ordering and interpreting various lab tests, but knowing when and which test to order is not always easy. As a general rule with any diagnostic testing, it is important to ask the following questions: “What am I looking for?” and “How will the results change the management of this patient?” The sensitivity, specificity, positive predictive value, and negative predictive values are all critical statistics that help you determine the answers to those questions (
Table 18-1
).
Table 18-1.
Calculations of Predictive Value, Sensitivity, and Specificity
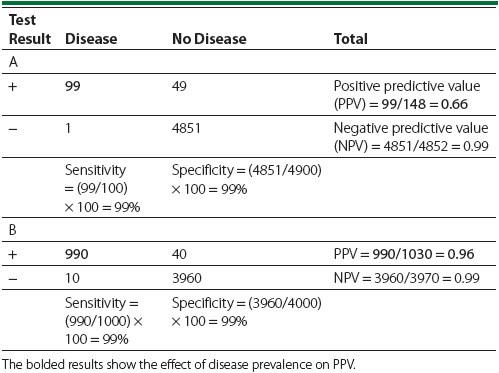
It should be noted that the positive predictive value and negative predictive values will be affected by the prevalence of the condition. Hence, when ordering tests for something very rare, the likelihood of a false test goes up. This is demonstrated in
Table 18-2
, where for the same specificity and sensitivity the positive predictive value increases dramatically as the disease prevalence goes from 2% in
Table 18-2
A to 20% in
Table 18-2
B. Awareness of such principles will maximize your likelihood of testing your patients appropriately.
Table 18-2.
Effect of Disease Prevalence on Positive and Negative Predictive Values
It is also important to note that laboratory tests that measure a continuous variable (eg, CBC, chemistries, LFTs) are subject to unavoidable systematic error intrinsic to the method by which the reference range is determined. For these types of tests the thresholds used to distinguish a “normal” result from an “abnormal” result are determined based on large samples of data from healthy
individuals, with the middle 95% of the values simply defined as normal. In other words, the reference range is calibrated for a specificity of 95%, which means that 5% of healthy individuals would be expected to have a falsely positive test result (ie, the result is outside the reference range even though they don’t have the disease). This has important clinical implications. If you order 20 tests (the labs included with a CBC with differential and a basic metabolic panel will generally cross this threshold), you should expect on average 1 value to be outside the reference range. Since “abnormal” values often lead to further testing, some of which are invasive, a false-positive lab test can be associated with substantial risk. While it may seem you are being more thorough when you reflexively order every lab available, taking the time to order only a limited number of labs is actually protective and is therefore better patient care.
