Resident Readiness General Surgery (25 page)
Read Resident Readiness General Surgery Online
Authors: Debra Klamen,Brian George,Alden Harken,Debra Darosa
Tags: #Medical, #Surgery, #General, #Test Preparation & Review

6.
What can be done to treat this patient?
7.
What is compartment syndrome?
ACUTE LIMB ISCHEMIA
Answers
1.
You first need to understand the pain: the quality, timing, location, onset, and severity. Has he had the pain before? Does he have associated numbness, tingling, or swelling? Does he have pain at rest? Has he ever had pain in the back of his calves, thighs, or buttocks associated with walking? Did it come on suddenly, or has it been worsening over the past few days? Is there any recent trauma to the area?
In terms of past medical history, a history of cardiac or vascular disease is key information: atrial fibrillation, angina/MI, claudication/ulceration, and transient ischemic attacks/strokes. Also notable is a history of cardiac or peripheral revascularization. Current medications are important, as is a personal or family history of cardiac disease, vascular disease, or a hypercoagulable state. Much of the past history gives you an idea as to the cause of ischemia, potential intraoperative challenges, and the perioperative risk associated with intervention.
This is also an appropriate time to gather a quick vascular-oriented review of symptoms. Questions should cover the carotids (visual changes, word-finding difficulties, transient ischemic attacks, or strokes with paralysis or paresthesias),
aorta (abdominal or back pain, family or personal history of abdominal aortic aneurysm [AAA]), and peripheral vasculature (claudication, rest pain, ulceration). This is by no means comprehensive, but remember that vascular disease involves numerous territories simultaneously.
On further questioning, Mr. P reveals that the pain behind his right calf started abruptly 5 hours ago. He has been able to walk around, but he notes that the leg is feeling weaker. His activity is so limited at baseline that he normally walks only a few blocks before becoming quite dyspneic. He notes no claudication otherwise, and his vascular review of symptoms is otherwise negative.
He has an 80-pack-year history of smoking, and he also has a history of atrial fibrillation. His warfarin dosing is managed by his PCP, but he takes it regularly with his last INR “above 2.”
2.
The lower extremity circulation begins with the common iliac artery. After the internal iliac branches, the external iliac comes forward and laterally within the pelvis and eventually crosses under the inguinal ligament. After the inferior epigastric and circumflex iliac arteries branch, it is called the common femoral artery (immediately proximal to the inguinal ligament). The next important branch point is the profunda femoris artery, which takes off posterolaterally from the common femoral artery to supply the thigh and deep muscles of the upper leg.
The superficial femoral artery continues and passes through the adductor (Hunter’s) canal. At the level of the adductor hiatus, it wraps behind the knee to become the popliteal artery, which is often referenced in relation to the knee joint, that is, above versus below the knee popliteal. Below the knee, the popliteal artery splits into 3 arteries (the “trifurcation”). The most common pattern begins with a 2-way split into the anterior tibial artery and the tibioperoneal (TP) trunk. The TP trunk then becomes the peroneal artery and the posterior tibial artery. All 3 of these arteries reach the foot: the anterior tibial artery runs laterally and eventually becomes the dorsalis pedis artery, the posterior tibial artery runs medially and can be felt behind the ankle (still called the posterior tibial artery), and the peroneal artery follows the fibula down to the ankle and bifurcates into medial and lateral branches, which provide collaterals to the foot.
The basic anatomy is fairly consistent (see
Figure 19-1
). Collateralization is crucial for patients with atherosclerotic disease, as it provides continued blood supply and also serves as a “detour” during acute occlusion. It is most commonly seen around major branch points: the external iliac filling through the pelvis (from the internal iliac artery), the superficial femoral artery reconstituting via the profunda femoris artery, and the foot filling through patent tibial vessels.

Figure 19-1.
Arterial circulation of the lower extremities. The left anterior tibial artery (arrow) is noted to be diseased. (Reproduced with permission from Brunicardi FC, Andersen DK, Billiar TR, et al.
Schwartz’s Principles of Surgery
. 9th ed. New York: McGraw-Hill; 2010 [Figure 23-59].)
3.
A pulse examination is essential. There are various scoring systems for pulses (0-2, 0-4, etc). If your scale may be unclear, document in words the pulse examination (easily palpable, barely palpable, dopplerable, etc). If unable to find a pulse by palpation, use a Doppler probe and note the characteristic of the sound. It is rare to have acute limb-threatening ischemia without a major pulse deficit.
If a patient has acute peripheral ischemia, the “6 P’s” are common examination findings: pain, pallor, poikilothermia (coolness), pulselessness, paresthesia, and paralysis. Paralysis is a late sign that warrants emergent intervention. Chronic ischemia is evidenced by hairless legs, symmetrically cool feet, dependent rubor, diminished pulses, and nonhealing distal ulcers or gangrene.
A commonly used measure of peripheral vascular disease is the ankle-brachial index (ABI). It is the ratio of the systolic blood pressure of the brachial artery to that of either the posterior tibial or dorsalis pedis artery. An ABI of 0.9 to 1.2 is considered normal. ABIs from 0.7 to 0.9 suggest mild disease, 0.7 to 0.4 imply moderate disease (usually associated with claudication), and less than 0.4 denote critical limb ischemia (rest pain). Of note, an ABI of greater than 1.2 signifies arterial calcification; in such instances, ABIs are not helpful. This is especially common in patients with diabetes and end-stage renal disease. Don’t let this fool you into thinking the patient has healthy arteries.
Back to our patient. On examination, you note the following pulses (see
Table 19-1
).
Table 19-1.
Mr. P’s Pulse Examination
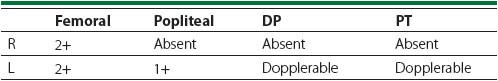
Mr. P’s right leg is notably cooler than the left, starting immediately above the knee. He has some small ulcerations on the first 3 toes of the left foot without evidence of infection, and there is a lack of leg hair starting halfway down the tibia bilaterally. He has weakness on movement of his right ankle, and his sensation is intact except for the web space between the first and second toes. His calves feel soft bilaterally. ABIs are >1.3 bilaterally.
From the examination you deduce that he has an acute arterial occlusion, likely at the level of Hunter’s canal. Your patient clearly has chronic peripheral vascular disease as well, indicated by weakened peripheral pulses, a history of claudication, lack of leg hair, and the ulcerations of the toes on the asymptomatic leg. He requires urgent revascularization of the right leg because of the acute ischemia.
4.
Basic laboratory workup is important, especially renal function tests, coagulation studies, creatinine kinase, and a urinalysis. Knowing the general function of a patient’s kidneys allows decisions about further imaging (CT angiogram, intraoperative angiogram, or duplex ultrasound). Creatinine kinase and a urinalysis are helpful when you suspect rhabdomyolysis associated with prolonged ischemia or compartment syndrome.
A complete blood count, coagulation studies, basic metabolic panel, and urinalysis are within normal limits except for the following:
INR 1.8
PTT 32.7
Cr 1.3
CK 10451
EKG atrial fibrillation with rate in the high 80s
Unfortunately, you have no other lab values for comparison purposes. The INR indicates that he is not therapeutically anticoagulated at this time. The elevated creatinine is indicative of underlying renal insufficiency and should be addressed by pretreatment with acetylcysteine (Mucomyst) and sodium bicarbonate. The elevated CK indicates ongoing muscle death from ischemia. His urinalysis is presently normal, but it will be important to closely monitor his urine for renal injury.
5.
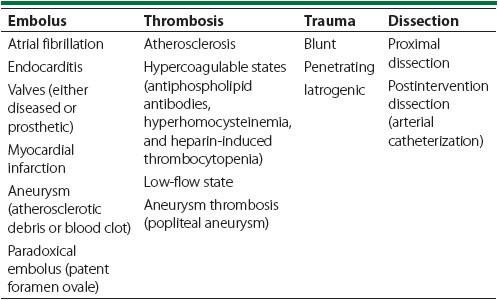
These are commonly divided into 4 categories: embolus, thrombosis, trauma, and dissection (see
Table 19-2
).
Table 19-2.
Common Causes of Acute Limb Ischemia
6.
After acute arterial occlusion is diagnosed, there are 2 priorities: systemic anticoagulation to prevent further propagation and urgent revascularization to reestablish blood flow to the extremities.
Anticoagulation is usually achieved with intravenous heparin (rather than low-molecular-weight heparin). Revascularization is simple in principle, but quite complicated in practice due to the myriad of options available. If clinically stable and appropriate from the standpoint of renal function, CT angiography is used to establish the level of the occlusion; simultaneously, the proximal and distal vasculature are assessed for other occlusions and possible bypass targets.
Thromboembolectomy is traditionally achieved by direct cutdown and embolectomy with Fogarty catheters. A lysis catheter with infusion of lysis agent (tissue plasminogen activator [tPA], urokinase, streptokinase, etc) can also be used in patients who have intact sensation and motor function, especially for patients in whom the risk of general anesthesia is felt to be high. Fogarty catheters can be used for embolectomy under local anesthesia as well.
All management decisions should be based on consultation with a vascular surgeon, and this depends on the acuity of presentation and anatomy.
Back to our patient. A CT angiography demonstrates an acute occlusion in Hunter’s canal. The length of the occlusion is relatively short, and there appears to be some reconstitution of flow below the level of the occlusion. Mr. P has single-vessel runoff to his foot via the posterior tibial artery. Because he is in atrial fibrillation and is subtherapeutic on warfarin, he is brought to the operating room for a direct cutdown and thromboembolectomy with Fogarty catheters. A lysis catheter is not entertained because he is having leg weakness with an elevated CK. The operation is successful in restoring flow to the foot, and completion angiography demonstrates good flow in the posterior tibial artery. On leaving, the posterior tibial pulse is now dopplerable.
7.
Compartment syndrome results from an ischemia–reperfusion injury after revascularization. This results in tissue swelling and entrapment by the fascia. This in turn can cause
more
ischemia by causing occlusion in extreme circumstances as the blood vessels are externally compressed. This results in more muscle death, release of myoglobin, and potential for renal injury and loss of the limb.
Other books
Wish Me Luck by Margaret Dickinson
Brave by Dawson, Zoe, The 12 NAs of Christmas
Along Came Merrie by Beth D. Carter
Mystery of the Stolen Boxcar by Charles Tang
Lumbersexual (Novella) by Leslie McAdam
Disobedience by Darker Pleasures
Submission by Ray Gordon
Plain Proposal by Beth Wiseman
Hot Properties by Rafael Yglesias
KISS THE WITCH by Dana Donovan
