Resident Readiness General Surgery (26 page)
Read Resident Readiness General Surgery Online
Authors: Debra Klamen,Brian George,Alden Harken,Debra Darosa
Tags: #Medical, #Surgery, #General, #Test Preparation & Review

There are 4 compartments of the leg: anterior, lateral, deep posterior, and superficial posterior. The anterior compartment is the most commonly affected (anterior tibial artery, deep peroneal nerve, and the 4 extensor muscles of the foot) (see
Figure 19-2
).
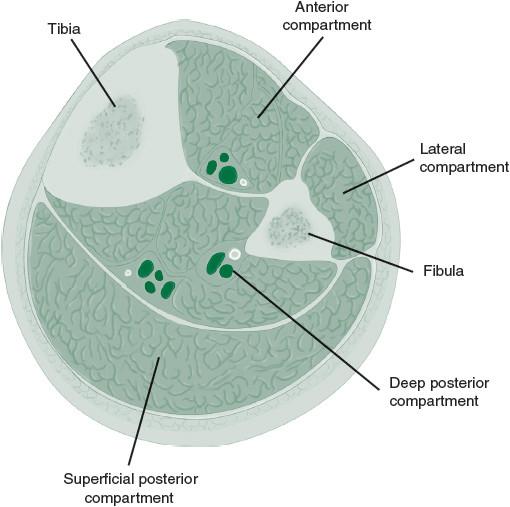
Figure 19-2.
Four fascial compartments of the lower leg. (Reproduced with permission from Brunicardi FC, Andersen DK, Billiar TR, et al.
Schwartz’s Principles of Surgery
. 9th ed. New York: McGraw-Hill; 2010 [Figure 23-62].)
Traditionally, compartment pressures greater than 30 mm Hg have been considered an indication for intervention. However, there are increasing data to suggest that the delta pressure (difference between diastolic pressure and compartment pressure) is a more accurate predictor of compartment syndrome. A difference of 20 mm Hg is the generally accepted value.
A 4-compartment fasciotomy can be performed by making an incision 2 fingerbreadths (4–5 cm) medial (deep and superficial posterior compartments) and lateral (anterior and lateral compartments) to the tibia. Once down to muscle, a long scissors can be used to split the fascia and assess the quality of the underlying muscle.
Back to the patient. Postoperatively, our patient’s pain is well controlled. At 4:00 the following morning, you are asked to evaluate him for worsening pain and an inability to move his right foot again. On examination, the arterial pulses are still dopplerable, but Mr. P notes weakness and numbness of the right foot. The calf feels “rock hard” and is tender to palpation, and you suspect compartment syndrome. Compartment pressures are measured at greater than 30 mm Hg. He is brought emergently to the operating room for 4-compartment fasciotomies.
Measuring the CK may or may not have been useful because of the recent operation. However, fasciotomies can be limb-saving and are indicated in this situation. Trending CK postoperatively after fasciotomies is common practice to ensure that there is no ongoing ischemia. Second-look operations are also common.
TIPS TO REMEMBER
Acute peripheral ischemia is a surgical emergency that can result in limb loss if not treated expeditiously.
Once the diagnosis is made, therapeutic anticoagulation is indicated. Further workup and planning is dictated by the clinical presentation, past medical history, health of the patient, and further imaging.
Compartment syndrome is also a surgical emergency managed by fasciotomies and conscientious wound care.
COMPREHENSION QUESTIONS
1.
Of the signs and symptoms of acute leg ischemia, which is typically the last one to occur?
A. Pain
B. Pallor
C. Poikilothermia
D. Pulselessness
E. Paresthesia
F. Paralysis
2.
What is the cutoff on ABI for critical leg ischemia?
3.
True/false: acute limb ischemia is associated with ulcerations.
4.
Which is
not
a fascial compartment of the leg?
A. Anterior
B. Lateral
C. Medial
D. Deep posterior
E. Superficial posterior
Answers
1.
F
. Paralysis is a late finding suggesting muscle necrosis and nerve injury, both of which take a substantial period of time. The other signs and symptoms tend to evolve much sooner.
2.
0.4
is the usual cutoff for critical limb ischemia, and it usually causes rest pain. This is time for either endovascular or open intervention to improve flow to the distal extremities to improve rest pain and/or prevent gangrene.
3.
False
.
Acute
limb ischemia is not associated with ulcerations unless superimposed on ischemia that is also chronically present. The chronicity of peripheral ischemia matters, especially when considering the appropriate intervention in the acutely cold extremity.
4.
C
. The medial compartment does not exist in the leg.
 A 36-year-old Woman Status Post Motor Vehicle Accident While Intoxicated
A 36-year-old Woman Status Post Motor Vehicle Accident While Intoxicated
Shamim H. Nejad, MD and Nadia Quijije, MD
A trauma alert is called for a 36-year-old woman brought in by ambulance after intentionally crashing her car into a tree while intoxicated. On physical examination, her vitals are: T 98.6, BP 165/80, HR 115, RR 16, O
2
88% on RA, and 96% with 3 L NC. She is slightly lethargic and disoriented to time, but able to answer simple questions. She complains of acute pain in her chest along with a mild headache. She displays no evidence of diaphoresis or tremor and denies feeling anxious or nauseated. Pupils are reactive, without any evidence of nystagmus. The remainder of the neurological and general examination is normal.
The patient gives a history of binge-type drinking, in which she consumes “a lot” of vodka every weekend. She denies daily drinking, however also reports that alcohol helps her sleep at night. She reports 1 previous detox approximately 1.5 years ago. She also notes losing 1 job in the past due to her alcohol use, along with it affecting past relationships, and legal complications due to assaulting others while intoxicated. She denies a history of past delirium tremens or alcohol withdrawal seizures. She denies any history of benzodiazepine, cannabis, cocaine, heroin, or other drug use.
Her injuries include multiple left-sided rib fractures and a subarachnoid hemorrhage for which she is started on levetiracetam (Keppra) for seizure prophylaxis. She is found to have a blood alcohol level (BAL) of 3600 mg/L in the emergency department, along with an AST of 235 U/L, an ALT of 120 U/L, and a normal mean corpuscular volume (MCV) of 95.
1.
Name 4 symptoms or signs of alcohol withdrawal.
2.
Is she at high risk of developing alcohol withdrawal syndrome (AWS)? How can you tell?
3.
What is the treatment of symptoms due to alcohol withdrawal?
4.
For a patient with AWS, when should psychiatry be consulted?
ALCOHOL WITHDRAWAL
Answers
1.
Long-term exposure to ethanol results in adaptive changes in several neurotransmitter systems. Abrupt withdrawal of ethanol results in nonphysiologic levels of these neurotransmitters, which in turn cause the signs and symptoms of alcohol withdrawal. Understanding the basics of these changes not only can help guide your choice of therapy but also can help you appreciate alarming versus less concerning signs.
The changes in neurotransmitter systems can be clustered as shown in
Table 20-1
.
Table 20-1.
Alcohol Withdrawal Symptom Clusters
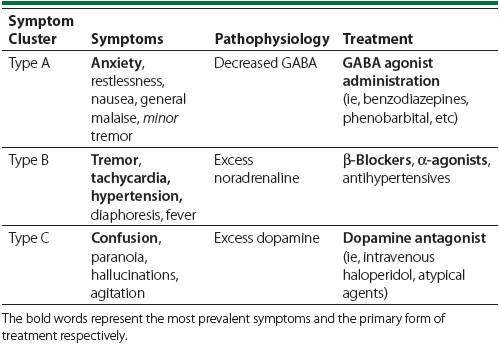
Chronic exposure to alcohol results in an increase in glutamatergic reaction and decrease in GABA activity. When alcohol is abruptly removed, decreased GABA activity leads to symptoms of anxiety and restlessness, referred to as
uncomplicated
AWS. Concomitantly, excess glutamate stimulates an increase in noradrenaline and dopamine, as shown in
Figure 20-1
. Increased noradrena-line results in Type B symptoms resulting in increased sympathetic activity (see
Table 20-1
). Increased dopaminergic activity leads to Type C symptoms, a contributor to alcohol hallucinosis and, in conjunction with severe Type B symptoms, delirium tremens (alcohol withdrawal delirium). Seizures, alcoholic hallucinosis, and delirium tremens are AWSs referred to as
complicated
AWS (see
Table 20-2
).
