Resident Readiness General Surgery (58 page)
Read Resident Readiness General Surgery Online
Authors: Debra Klamen,Brian George,Alden Harken,Debra Darosa
Tags: #Medical, #Surgery, #General, #Test Preparation & Review

2.
C
. In order to replete her sodium, it is imperative to determine her actual sodium deficit. Using the equation for Na deficit (0.55 [weight in kg] × [140—serum Na]), her total Na deficit is 385 mEq. Using 0.9% NS for repletion (which has 154 mEq of Na per liter), she would require 2.5 L (385/154) to make up for her sodium deficit.
3.
B
. Calcium gluconate is the initial treatment of acute hyperkalemia. It stabilizes the myocardium, but is temporizing with effects lasting only 30 minutes. Insulin is also a rapid-acting and temporizing measure, but is second line. Both Kayexalate and dialysis are definitive treatments for hyperkalemia, and should be instituted as soon as the hyperkalemia has been acutely corrected with more rapid measures.
 A 58-year-old Man With a Postoperative Fever
A 58-year-old Man With a Postoperative Fever
Jahan Mohebali, MD
You are paged about a fever of 101.8°F in a 58-year-old man who is postoperative day 3 from a colostomy reversal. He is normotensive, his heart rate is 110, and while he is oxygenating well, he is breathing at 22 breaths/min. His past medical history is notable for COPD and his preoperative medications include 4 mg of oral prednisone taken daily. This is the first fever that he has had since the operation and his nurse is requesting that you order Tylenol. When you evaluate the patient at the bedside, he states that he “doesn’t feel too well.”
1.
Based on the timing of the patient’s fever, would you be surprised if he is ultimately diagnosed with a pneumonia?
2.
What history and physical exam findings will help to confirm the diagnosis?
3.
What are the initial steps in the workup of postoperative fever?
4.
Other than pneumonia, what other factor may be responsible for the patient’s tachypnea and fever?
5.
What are the initial steps in empiric treatment of this patient’s fever?
6.
Should the patient receive acetaminophen (Tylenol)?
POSTOPERATIVE FEVER
A surgical fever is defined as a temperature greater than 101.5°F or 38.5°C. The major etiologies for postoperative fever that should always be considered include atelectasis, pneumonia, urinary tract infection, intra-abdominal infection or leak, wound infection, and deep venous thrombosis. Other processes such as malignant hyperthermia, superficial thrombophlebitis,
C. difficile
colitis, endocarditis, and line infections should also be considered given the appropriate circumstances.
It is often helpful to categorize these various etiologies by the postoperative day on which they are
most likely
to occur (see
Table 44-1
). It is, however, important to note that any of these processes can occur on any postoperative day.
Table 44-1.
Most Likely Fever Etiology by Postoperative Day
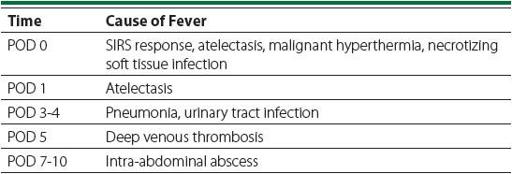
POD 0 to 1
: There are multiple possible causes of fever on POD 0 and 1, including malignant hyperthermia, necrotizing wound infection, systemic inflammatory response syndrome (SIRS), and atelectasis. While atelectasis has traditionally been considered the most common cause of fever on postoperative day 1, it is a diagnosis of exclusion and more serious etiologies should be ruled out. These include malignant hyperthermia that is most likely to manifest in either the operating room or the PACU, and a severe necrotizing wound infection. Therefore, even if atelectasis is suspected, the patient should be examined and the dressing should be removed in order
to inspect the wound. Within the first 48 hours post surgery the dressing removal should be done in a sterile fashion.
If more serious causes have been ruled out, the fever is most likely due to a postoperative SIRS response or atelectasis. If you suspect the latter, then treatment is simple and consists of aggressive incentive spirometry, encouraging coughing and deep breathing, and ambulation.
POD 3 to 4
: Classically, this is the time that urinary tract infections and pneumonias first manifest. Again, however, it should be noted that this time frame is not absolute. For example, an aspiration pneumonia related to intubation will probably present earlier, and a patient may present to the hospital already having a UTI. Nonaspiration pneumonias typically result from inadequate pulmonary toilet, and postoperative UTIs are often secondary to Foley catheter insertion or failure to remove the Foley catheter as early as possible. A final etiology that should always be considered in patients who have undergone abdominal surgery is an anastomotic leak that can manifest as fever as early as POD 3.
POD 5
: Deep venous thrombosis. Surgery increases the risk of deep venous thrombosis. These clots can be a nidus for inflammation and infection.
POD 7 to 10:
Intra-abdominal abscess. It takes a while for the bacteria to multiply and for the body to react.
It is important to remember that any source of infection can lead to bacteremia, or sepsis. Although a full discussion of the SIRS response and sepsis is covered in other chapters, the astute clinician should always be looking for systemic signs of infection whenever presented with a patient with postoperative fever.
Answers
1.
The patient in the case above is experiencing a fever on postoperative day 3. Given his concomitant tachycardia and tachypnea, there should be concern for pneumonia or a more serious infection with systemic effects. In this case, given
his specific operation and his preoperative steroid use, there should also be a higher-than-usual suspicion for an anastomotic leak.
2.
The junior surgical resident will often encounter postoperative fever when paged by a member of the nursing staff. Although it may be tempting to simply order Tylenol and address the issue later, particularly if the page occurs in the middle of the night, the patient should always be evaluated at the bedside. A brief history focusing on symptoms such as dyspnea, sputum production, worsening abdominal pain, leg pain, diarrhea, or urinary frequency and burning should quickly be obtained. A physical exam should include auscultation of the lungs, an abdominal exam, an exam for leg edema or pain with passive motion (Homans’ sign), and palpation of the calves for “cords” suggestive of DVT. Finally, the patient’s primary dressing should be removed in order to evaluate the wound.
3.
After a brief history and physical exam, a diagnostic workup should be initiated based on the postoperative day as well as any other patient-specific factors (see
Figure 44-1
). Often, no additional workup is needed in the first 24 hours in an asymptomatic patient assuming that the serious causes of fever in this time period have been ruled out as mentioned above. After the first 24 hours, minimal workup should include a complete blood count with differential, urinalysis, chest x-ray, and 2 sets of blood cultures drawn from separate sites. Depending on the patient’s symptoms or chest x-ray findings, a sputum culture and duplex venous studies may also be obtained. In general, the decision to obtain additional imaging such as an abdominal CT scan to look for an anastomotic leak or intra-abdominal abscess should be made in conjunction with the senior resident or attending.
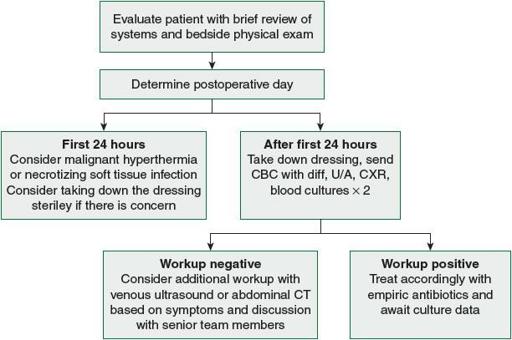
Figure 44-1.
Algorithm for evaluating postoperative fever.
4
. Although respiratory symptoms such as tachypnea may simply indicate an underlying pulmonary process such as pneumonia, they should also raise concern for a severe infection or impending sepsis. A portable chest x-ray is very useful to help differentiate among the possibilities.
5.
If you suspect an infection, workup should proceed as above with the goal of identifying a target for possible antibiotic treatment. If no target can be identified (ie, the patient has a fever of unknown origin), then a decision must be made regarding initiation of empiric treatment. That decision will be made in consultation with either your senior resident or attending, and will typically integrate factors such as patient symptoms, hemodynamics, and overall risk of complications.
In this case, the patient is 3 days into a hospital course, has COPD, and is on prednisone suggesting that broad-spectrum coverage for pneumonia should be employed. A good regimen would be vancomycin, Zosyn, and levofloxacin.
6.
Although acetaminophen (Tylenol) is beneficial for the symptomatic treatment of postoperative fever, its downsides are 3-fold. Most seriously, high doses of acetaminophen are hepatotoxic. More subtly, it is often clinically useful to follow a patient’s fever curve as a marker of adequate source control, and the use of acetaminophen can obscure these data. Lastly, fevers are a physiologic response to infection that change the temperature of the culture medium (ie, the patient) for bacteria that are adapted to reproduce best at normal body temperatures. Medically “correcting” this mild hyperthermia therefore is of benefit mostly to the bacteria—it is unlikely to augment either the doctor or the patient’s ability to resolve the infection.
For all of these reasons it is best to avoid reflexively treating a fever with acetaminophen, but instead reserve it for those cases where the patient is dangerously hyperthermic or if the fever is especially symptomatic.
TIPS TO REMEMBER
The etiology of postoperative fever is often related to the specific postoperative day on which the fever occurs:
POD 0 to 1: atelectasis:
